One
Important points
●Exclusive breastfeeding is recommended from birth to 6 months of age (up to 180 days of age);
● When the amount of breast milk is insufficient, infant formula can be supplemented;
● Vitamin D supplementation of 400 IU (10 micrograms)/day, without calcium supplementation, is started a few days after birth (after delivery and discharge);
● Identifying infant hunger and satiety signals, and parents responding in a timely manner is the key to establishing good eating habits early;
● Correct use of growth curves to regularly evaluate the nutritional status of infants.
(1) Feeding recommendations
1
Exclusive breastfeeding
Breastfeeding is given as early as possible after childbirth, and breast milk is the best food source for babies after birth. Exclusive breastfeeding means that breast milk is the only food source for babies, in addition to essential medications, vitamin and mineral supplements, and does not eat any other liquid and solid foods, including water. Breast milk contains 88% water, and proper and adequate breastfeeding can adequately guarantee the water needs of babies under 6 months of age, even in hot weather, as long as the breast milk is adequately fed without additional water.
2
Formula feeding
Breast milk is the best source of nutrition for babies, but formula can be used when the mother is unable to breastfeed her baby for various reasons. Neonatal formula feeding should also be given as needed, gradually increasing, and meet their energy needs when ingestion of formula is about 20 g/(kg·d) or 150 ml/(kg·d). At the same time, it should be noted that the amount of milk intake of the same infant can fluctuate every day, and different individuals also have certain differences.
3
Breastfeeding nutrition
Nursing mothers should adhere to a balanced diet, daily energy intake should be increased than usual, there are large individual differences in the amount of increase, generally an increase of 2 092 kJ per day (equivalent to 500 kcal, 1 kcal = 4.184 0 kJ) energy (equivalent to an additional meal) can ensure that it produces enough milk to feed the baby. Mothers should continue vitamin and mineral supplementation during pregnancy during breastfeeding. The amount of breast milk and the concentration of protein, fat and lactose in it are not affected much by the mother's diet, but the level of micronutrients and fatty acids is significantly affected by the mother's diet. Healthy mothers with a balanced diet who consume deep-sea fish once or twice a week can basically guarantee the level of docosahexaenoic acid (DHA) in their milk, without the need to take additional supplements [4]. If the mother is malnourished or vegetarian, additional DHA supplementation is required in addition to multivitamin supplementation. To avoid excessive mercury intake, pregnant women should avoid large, meat-eating fish. Vegetarian mothers should also supplement with vitamin B12. Babies can feel the taste of different kinds of food through milk, so it is beneficial for the mother to eat different kinds of food to facilitate the baby to receive different kinds of solid food later.
4
Vitamin & Mineral Supplement
(1) Vitamin D and calcium: Regardless of the feeding method, it is recommended to start vitamin D supplementation after the newborn is discharged from the hospital, and the recommended dose for term infants is 400 IU (10 μg) per day without calcium supplementation [5].
(2) Vitamin K: Within 6 h after birth, it is recommended to inject 1.0 mg of vitamin K intramuscularly to prevent vitamin K deficiency hemorrhage [4].
(2) Recommendations for eating behavior
Breastfeeding tips
Breastfeeding should be started as early as possible in the postpartum period (
Number of breastfeedings
Encouraging breastfeeding on demand is especially important for establishing and maintaining good breastfeeding practices early. Breastfeeding on demand means that the frequency and duration of breastfeeding are not limited when the baby is properly breast-sucking. Infants aged 1 to 2 months are advised to wake up and feed them during the day for 4 hours to avoid inadequate milk intake [8]. The interval between nighttime breastfeeding may be extended, about 3 hours, or 4 to 5 hours. The number of breastfeeding sessions in 24 h is 8 to 10. Newborn babies may have a long time with nipples (feeding > 30 min/time) or too much feeding frequency (1.0 to 1.5 h feeding) because they are not yet suitable for out-of-home life, which is on-demand breastfeeding. Breastfeeding can generally be gradually and regularly after 2 months of age, and improper sucking or disease should be ruled out if there is insufficient growth. Cleft nipples in mothers are also often associated with incorrect suction posture. Once a nipple crack occurs, a small amount of milk can be expressed and spread evenly on the nipple after each breastfeeding.
Bottle feeding posture
When feeding a baby, the upper arm should be used to support the baby well so that it feels comfortable and safe, the head and body are in a straight line, and the bottle should be held and have good eye contact with the baby during feeding. Avoid letting the baby drink milk with the bottle in the absence of support, which is prone to coughing, ear infections, and caries after the baby's teeth are cute.
Bottle cleaning, formula preparation and storage
Bottles and nipples need to be thoroughly cleaned and sterilized after each use, and can be disinfected with special disinfection equipment or boiled in boiling water for 5 minutes. Clean the area and wash your hands thoroughly with soap before mixing the powder. Ensure hygienic drinking water for milking and apply boiled and cooled water. Prepare formula milk in strict accordance with the instructions, add water and then add milk powder when brewing, and weigh the milk powder with the measuring spoon matching in the jar to avoid excessive dilution or excessive thickness caused by infant malnutrition or kidney damage. Place a few drops on the inside of your wrist before feeding to make sure the milk is at the right temperature. The remaining liquid milk can be stored in the refrigerator and eaten next time it is warmed and mixed with the newly prepared milk. Formula that has been left for more than 1 h at room temperature or has been warmed once should be discarded.
5
Identify infant hunger and satiety signals
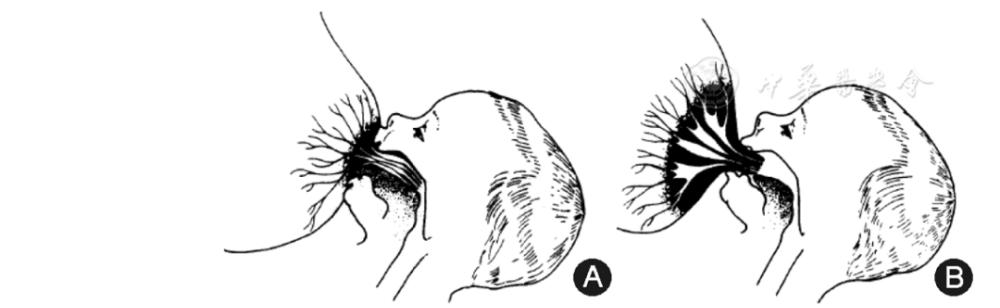
Timely response is key to establishing good eating habits early on. Newborns may have foraging reflexes, sucking movements, or dancing hands when they are hungry; babies may have hands in their mouths and suck, grimace, irritability, and loud crying are the last signs of hunger. The expressions and movements of infants at different stages of hunger are shown in Figure 2. Caregivers should pay attention to the early signs of infant hunger and avoid feeding after crying, which will increase the difficulty of feeding, especially in breastfed babies, and crying can affect the sucking of the mother's nipple. Babies stop sucking, open their mouths, turn their heads away, etc. often represent a feeling of fullness and do not force food again.
(3) Common problems and handling
Milk spillage
During or after feeding, the baby's head should be lifted upright on the mother's shoulder and patted on the back to help drain the swallowed air and prevent milk leakage. Infants should sleep in the right lying position to prevent choking due to milk leakage during sleep. If necessary, the intake of milk can be reduced by 20 to 30 ml. If there is no improvement in the symptoms of milk leakage or poor weight gain in infants after guidance, it should be referred for further diagnosis in time to rule out organic disease.
Pacifier
Pacifiers are not recommended for newborns up to 1 month of age, as they may affect the establishment of breastfeeding habits and lead to premature weaning. If the pacifier is used later, it is necessary to avoid the establishment of a bad conditioning reflex between the use of the pacifier and the falling asleep behavior, and rely on the pacifier to re-fall asleep after waking up at night, which will affect the development of good sleep habits in the baby and lead to frequent night awakenings. It is not recommended to apply syrup or honey, etc. to the pacifier to soothe the baby.
Eat and sleep
Newborn babies have a high proportion of sleep time, and the circadian rhythm is not yet well established, so most of them will have the habit of eating and sleeping. However, most infants have established a relatively fixed diurnal rule since the age of 3 months, whether breastfeeding or formula feeding should avoid sleeping while eating, the feeding process should be an opportunity for parent-child interaction. It is appropriate to feed the time in advance, feed the baby in a relatively awake state, and when the baby has a sleep signal (rubbing his eyes, yawning, etc.) but has not yet fallen asleep, he will be placed on the bed to cultivate his independent sleep habit. In addition, pumping while sleeping is also prone to suffocation, which is not conducive to infant oral health care.
Maternal medication or alcohol and tobacco intake
When the mother takes most of the medications, it does not prevent her from continuing to breastfeed the baby. Mothers taking amphetamines, ergotamines, chemotherapy drugs, statins, sedatives, antiepileptic drugs, etc., it is recommended not to breastfeed for the time being, which can be detailed in the instructions of various drugs. Mothers should smoke as smoking increases the risk of respiratory allergies and sudden infant death syndrome in infants, as well as milk production and poor weight gain in infants. Alcohol can reduce the sensitivity of infants to the "ejaculatory reflex" caused by sucking, reduce lactation, and also adversely affect the baby's motor development, so it is recommended that mothers do not drink alcohol or alcoholic beverages. Mothers should limit their intake of caffeinated beverages (such as coffee, tea, and caffeinated beverages) to 2 cups per day.
Feeding after the mother goes out or starts working
Encourage mothers who go out or after work to breastfeed, breastfeeding no less than 3 times a day, and expressing breast milk when going out or at work to maintain the amount of breast milk produced. If there is too much milk during breastfeeding, it can be pumped out with a breast pump and stored in a special "milk bag". Breast milk after expression should be properly stored in the refrigerator or ice pack, the storage time of breast milk at different temperatures can refer to the following table, and it can be fed with warm water to about 40 °C before eating, avoiding using microwave heating milk (Table 1).
6
Situations where mothers should not breastfeed[10]
(1) The mother undergoes chemotherapy or radiation therapy;
(2) Serious heart, kidney and liver diseases, hypertension and diabetes with damage to the function of important organs, severe psychosis, recurrent epilepsy;
(3) When suffering from various types of infectious hepatitis in the acute stage, active stage of tuberculosis, epidemic infectious diseases, it is not advisable to breastfeed. Instead of feeding with formula, breast milk can be regularly pumped out with a breast pump to prevent milk return, and when the mother is cured and the infection period has passed, breastfeeding can continue;
(4) People suffering from breast herpes should not breastfeed;
(5) Drug-addicted mothers should not breastfeed before they have quit drugs;
(6) Mothers who are AIDS or infected with HIV should not breastfeed.
(4) Nutritional evaluation
Evaluation of feeding status
Ask about feeding to understand your baby's daily milk intake, frequency and timing of feeding, and nutrient supplementation. If possible, it is best to observe the mother feeding the baby on site. Adequate breastfeeding can be assessed by recording the number of diapers (diapers) in infants with adequate diapers in the first few weeks of life, and infants with adequate breast milk are wet with approximately 6 to 8 diapers per day (diapers are not wet). Early infants can have stools every time they change their diapers, or they can have a bowel movement every 2 to 3 days. Usually, breastfed babies have thin, yellow, mushy stools, but occasionally there are flaps and greenish colours, which are normal and need to be distinguished from diarrhea. At the age of 6 to 3 months of age, the frequency of bowel movements in breastfed infants begins to decrease, but the frequency of bowel movements varies widely, with some babies still having multiple bowel movements on 1 day or each day apart.
Early postnatal weight evaluation
Newborns lose about 6% to 9% of their physiological weight 1 week after birth, usually returning to their birth weight on the 7th to 10th. However, if weight loss exceeds 10% of birth weight, close follow-up and referral if necessary.
Nutritional evaluation is performed using growth curves
Parents are instructed to learn to use growth curves, and the results of monthly measurements are marked on the growth curve chart, and the nutritional status of infants is monitored by comparing with the growth data of infants of the same age and sex, focusing on the weight of age, the length of age and the weight of length. If the relevant measurement on the growth curve is less than the 3rd percentile or greater than the 97th percentile, or if the index rises or falls across the 2 major percentile curves compared with the previous assessment, attention should be paid to and referral should be made in a timely manner if necessary. For specific methods of physical growth evaluation, see "Recommendations for The Evaluation of Growth in Chinese Children" [11].
2. 6 to 8 months of age
Breast milk remains the most important source of nutrition for infants at this stage;
● Insist on breastfeeding and introduce solid foods rich in iron, such as iron-fortified rice flour or red meat foods rich in iron and zinc;
● The gradual transition of solid food to crumbled form helps babies learn to swallow and chew, while ensuring the energy density of food;
● Infants still need vitamin D 400 IU (10 micrograms) /day supplementation, and no calcium supplementation is required under the guaranteed milk level;
● Correct use of growth curves to regularly evaluate the nutritional status of infants;
● Routine blood tests at 6 months of age to screen for iron deficiency anaemia.
breastfeeding
Breastfeeding supplemented by iron-rich solid foods remains the best source of nutrition for infants at this stage and continued breastfeeding until age 2 should be encouraged. At this stage, the baby's need for breast milk should still be met as much as possible, and breast milk should account for 2/3 of the baby's daily energy supply during the 6 to 8 months of age. Breastfeeding infants in particular requires attention to iron nutrition.
It is recommended to choose formula milk, the amount of milk is 700 ~ 900 ml /day. Since formula-fed infants have a higher basal energy metabolic rate than breastfeeding, their energy needs are slightly higher than those of breastfeeding. The number of feedings in 24 h is about 5 to 6 times, and during the disease state and disease recovery period, the energy demand will increase, and the number of feedings needs to be appropriately increased. Formula-fed infants require more extra water than breastfeeding, especially during the hot season.
Solid food added
The food introduced should be mainly iron-fortified foods, iron-fortified cereals such as rice flour are the first foods introduced, and rice flour can be mixed with breast milk or formula. When semi-solid or solid foods are added early, each additional food should be observed for 3 to 5 days to see if the baby is adapted. Gradual addition of fruits, vegetables, meat, etc., especially red meat foods can be a good supplement to the iron and zinc that babies need. Animal livers are a good source of iron, but since the liver is a detoxification organ, some toxic substances tend to accumulate here, so it is not recommended to add too much [8]. In areas where iron-fortified cereals are not available, the addition of iron and zinc-rich animal foods (red meat, poultry eggs, fish) is particularly important and can be added starting with red meat puree. Solid foods introduced avoid salt, sugar, and other seasonings. Add food to gradually transition from puree to crumbs to help babies learn to chew and ensure the energy density of the food.
(1) Vitamin D and calcium: Regardless of the feeding method, infants still need to supplement with 400 IU (10 micrograms) of vitamin D per day without calcium supplementation [5].
(2) Iron: Exclusive breastfeeding or breast milk is mainly term healthy infants if the addition of solid food is reasonable (such as 30 grams per day rich in iron rice flour), in general, there is no need to add additional iron. 500 ml of iron-fortified formula guarantees the baby's basic iron needs.
Establishment of interactive feeding methods
Early establishment of interactive feeding patterns has important implications for the long-term eating behavior of infants and young children. When feeding solid food, place the baby in a safe, comfortable dining chair to ensure that their head, torso and feet are well supported. The hands should be free to move and interact well with the feeder. The feeding process is a parent-child interaction process in which the feeder actively responds to the infant's hunger signal and actively encourages the infant to eat during the feeding process. Avoid distractions when feeding, such as watching TV, playing with toys, etc. There is adequate eye contact and verbal communication with the infant during feeding, which promotes emotions. When a baby refuses a newly added food, do not force it to eat, you can try again, sometimes the baby needs to go through 10 to 15 experience attempts before accepting a new food.
Meal times
Eat milk 4 to 5 times and cereal-based solid foods 1 to 2 times. The frequency of solid foods can be gradually increased, and the amount of solid food ingested varies individually, and the amount of each consumption is based on the principle of not significantly affecting milk intake. The frequency of eating is related to the energy density of food, and the frequency of thinner foods needs to be higher, and the frequency of eating is relatively less. In general, the energy density of solid foods should be higher than that of breast milk to avoid poor growth due to insufficient energy.
Food preparation clean request
Ensuring a clean food preparation process is an important measure to prevent intestinal infections, including washing hands with soap beforehand, eating food as soon as possible after it is finished, using clean dishes, and paying attention to drinking water. Avoid feeding food that has been exposed to adult oral saliva to the baby, and avoid spreading bacteria from the adult mouth to the baby, causing caries.
It is recommended to gradually stop feeding infants at night
Infants aged 4 to 5 months have a mature digestive tract and can consume enough milk during the day to ensure their growth, so they do not need to be fed at night. Multiple night feedings not only affect regular daytime eating, but also affect the quality of the baby's sleep. Attachment emotions develop in infants aged 4 to 5 months, and breastfeeding-related conditioning reflexes (mother's body odor, milky taste, voice, etc.) have been established, and it is recommended that infants sleep in separate beds with adults, which can dilute the conditions related to breastfeeding. By gradually reducing the amount of each feeding, gradually postponing each feeding time, and finally stopping night feeding.
Method for adding paste-like solid food
Solid foods should be fed with a spoon instead of a bottle, and babies will cough, vomit or extend their tongue when they start eating solid food, but this phenomenon will gradually decrease as they continue to experience eating with a spoon and the ability to swallow. At this stage, the infant should also be gradually exposed to the use of the cup, which can be gradually introduced by evaluating the infant's development level. When the baby sits alone and can thumb-palm grasp, start to let the baby try to drink water with the cup; when the baby starts thumbnaking, like to try to hold the cup by himself, although he can't yet master the technique of drinking milk or water from the cup, he can still start trying to feed the baby a small amount of breast milk, formula or water with the cup.
Reasons for not gaining weight or significantly slowing down the growth rate
After starting to add solid foods at 6 months of age, if the addition is not appropriate, it is easy to cause weight loss or a significant slowdown in growth. The most common reason is that too much solid food (including amount and frequency) leads to a significant reduction in milk production, and the energy density of solid food is insufficient (too much water content), resulting in poor baby weight growth. Therefore, it should be emphasized that the addition of solid food at the age of 6 months is to add the part of the energy deficiency and the iron element that is most likely lacking through the solid food under the condition of basically maintaining the original milk amount, while training the infant to chew and swallow.
The age at which the seasoning was added
In order to avoid excessive salt (mineral) intake of infants to increase the burden on the kidneys, it is generally not recommended that infants under 1 year of age add sugar, salt and other seasonings during the preparation of food. However, if the food is mainly carbohydrates in poor areas, a small amount of oil can be added to increase the energy source of food.
The difference between fruit and juice
Fruit is one of the 5 main food types of the dietary pyramid. At 6 months of age, you can gradually start adding fruit, starting from the puree and gradually transitioning to small fruit grains. Some guidelines before 2010 also recommend that after 6 months, you can add a small amount of freshly squeezed juice and 100% pure fruit juice. However, due to the lack of fiber rich in fruit juice, and the increase in the burden on the digestive tract of infants affecting milk intake and increasing sugar intake, feeding guidelines in many countries in recent years do not recommend that infants under 1 year of age be fed juice [6,12].
At this stage, solid food is introduced, which is more likely to cause poor weight gain and nutrient deficiency due to improper feeding, so it is necessary to ask about daily milk intake and understand the addition of solid food, including type, texture, frequency and feeding method.
Growth evaluation
Infants grow faster at this stage
Screening for anemia
Routine blood tests are performed at 6 months of age for anaemia, and iron deficiency and iron deficiency anemia are predisposed to occur when feeding inappropriately at this stage, as detailed in the "Guidelines for the Prevention and Treatment of Iron Deficiency and Iron Deficiency Anemia in Children" [13].
3. 9 to 11 months of age
●Milk remains the main source of nutrition for infants;
● Intake of foods rich in iron and zinc, food varieties should be gradually diversified, gradually transition to adult food;
● During the critical period of food-to-material conversion, infant learning to chew and self-feeding, improper feeding can easily lead to various eating behavior problems in early childhood;
● Screening for iron deficiency anemia at 12 months of age.
(1) Nutritional recommendations
Breast milk in combination with other solid foods is the best nutritional match for babies and encourages able mothers to continue breastfeeding until age 2. The frequency of breast milk intake in infants aged 9 to 11 months is reduced, but due to the increase in each intake, the total daily breast milk intake is close to that of 6 to 8 months of age. As weight increases, the part that needs to be increased in energy intake should be satisfied by increasing the energy density and amount of solid food.
The amount of milk for infants at this stage is 700 to 900 ml per day, 4 times every 24 hours. Formula-fed infants require more water intake than breastfed infants, especially during the hot season, but only if they do not significantly affect milk intake.
The variety of food categories should be more abundant than in the previous stage.
(2) Iron: This stage is still a high incidence of iron deficiency anemia, and it is still necessary to pay attention to the nutritional status of iron. Breastfed infants with adequate additions to iron-rich solid foods or infants fed more than 500 ml of formula generally do not require additional iron supplementation.
Learn to eat on your own
It doesn't have to be required to use the tableware correctly, allowing active grasping of food to be self-feeding, which helps to master independent eating skills faster and develop self-confidence. When babies eat themselves, parents should tolerate spillage and messing, and can lay corresponding mats on the ground in advance to facilitate cleaning.
Learn to swallow and chew
This age stage is a critical period for cultivating infant chewing function, and different textures of food (including crumbs, granules, lumps, etc.) can help infants gradually learn to swallow and chew food, effectively reducing common eating problems in early childhood (such as food in the mouth for a long time, difficulty swallowing fiber, slow eating, etc.). Eating different textures of food separately, such as rice and vegetables, and avoiding soup rice can help babies learn to chew different textures of food.
Meal arrangements
Most 9-month-old babies can be consistent with the family's meal time, that is, three main meals in the morning, middle and evening, mainly milk, and then add 2 to 3 complementary meals, mainly solid food. Infants may eat different amounts each time, such eating arrangements can give babies the opportunity to contact different types of food to ensure adequate nutrition, complementary meals are a good opportunity to add new food, do not have to force the baby to eat the same amount each time, allowing food fluctuations. Help babies start using cups, and 12-month-old babies can drink water from a straw cup.
Solid food additions are associated with deciduous tooth eruption
Infant teething morning and evening have a very obvious individual difference, this stage of the addition of solid food, especially the conversion of solid food should not be based on toothing as the basis for the conversion of food and matter. Because, at this stage, babies usually use their jaws and tongue to chew and chew and crush various foods. The conversion of food and material land should be more according to its actual monthly age, and its development level can be referenced. 6 to 8 months of age should gradually transition from mushy food to granular food, about 8 months of age, most babies can use their fingers to grab solid food and send it to the mouth, can be fed lumpy food, also known as finger food (food that can be picked up with fingers). Around the age of 12 months, it should gradually approach the texture of adult food.
Feeding of sick infants
When the infant is ill, the feeding process should pay attention to appropriately increasing fluid intake and giving easily digestible and absorbed foods. After recovering from the disease, more food should be given than usual to help replenish the energy consumed too much due to the disease.
100% fruit juice is different from juice drinks
At this stage, it is still recommended to give infants flaky or lumpy fruits, even if a small amount of juice is given to infants, it should be freshly squeezed juice or 100% juice, rather than juice drinks. Fruit juice drinks refer to drinks with a juice content of 10% to 99%, and sweeteners, flavors, and sometimes vitamin C or calcium, which are not recommended for infants and young children. Similarly, sugary drinks containing dairy or probiotic ingredients are not suitable for infants and young children.
Infants are asked about daily milk and solid food intake, food-to-substance conversion, infant chewing food, and development of self-feeding skills.
Focus on the weight of age, length of age, and weight of length, see "Recommendations for The Evaluation of Children's Growth in China" [11]. Use growth curves to assess infant growth levels, velocities, and uniformity. If the relevant measurement is in the 97th percentile on the growth curve, or if the indicator is up or down across two major percentile curves compared to the previous assessment, the cause needs to be sought and referred as necessary.
Routine blood tests are performed at 12 months of age to understand iron deficiency, and iron deficiency and iron deficiency anemia are predisposed to improper feeding, as detailed in the "Guidelines for the Prevention and Treatment of Iron Deficiency and Iron Deficiency Anemia in Children" [13]. Patients with poor treatment should be referred.
4. 12 to 36 months of age
● After the age of 1, you should choose easily digestible home-cooked food, the food is suitable, a small amount of salt and oil can be added, and the regularity of eating is consistent with the family;
● Conditional mothers (adequate milk, non-attachment in children) can continue breastfeeding until 2 years of age;
● Pay attention to eating behavior training, develop good eating habits, avoid partial eating and picky eating behavior, and should get out of the bottle after 15 months of age;
● Young children should consume vitamin D 400 to 600 IU (10 to 15 micrograms)/day, including food and vitamin D supplement sources.
● At least 500 ml/day milk amount to ensure calcium nutritional requirements;
● Correct use of growth curves to evaluate the nutritional status of young children;
● Routine blood tests are performed annually to screen for iron deficiency anaemia and to prevent iron deficiency anemia.
Young children's growth rate is significantly slower than in infancy, appetite fluctuates greatly, sometimes even less than infancy, but the intake of food is thicker and the energy density is higher than in infancy.
Variety of food
The energy supply structure of food in early childhood has changed significantly, the food types are basically the same as adults, the proportion of energy provided by fat has decreased, and the proportion of carbohydrates has gradually increased (cereals 100 to 150 g/d, vegetables 200 to 250 g/d, fruits 100 to 150 g, meat animal foods 50 g/d, milk at least 500 ml/d). Eligible mothers continue to breastfeed until the age of 2. Children are not required to eat all foods, but they need to ensure the intake of each large type of food, such as not necessarily eating a variety of green leafy vegetables, but need to eat at least 1 to 2 kinds of vegetables. Like adults, normal young children can prefer one or more foods, but control the amount of food they prefer, and provide other healthy foods to ensure that the child is nutritionally balanced. If only the preferred food is provided, it is easy to form a picky eating habit in children. Encourage young children to drink water appropriately, but not drinks.
Food-eating land
Food of different textures can further train young children's ability to swallow and chew. To prevent young children from choking, avoid eating nuts, or granular foods that are prone to aspiration, such as peanuts, corn, grapes, jelly, etc.
Vitamin and mineral supplements
(1) Vitamin D:
In 2008, the American Academy of Pediatrics and the Chinese Journal of Pediatrics published recommendations on vitamin D recommendations in 2008 and 2010 recommended 400 IU (10 μg) for children over one year of age [14,15,16]. However, the 2016 Global Evidence-Based Guidelines for the Prevention and Treatment of Nutritional Rickets, building on global research evidence, recommend that children over 1 year of age receive 600 IU (15 μg) of vitamin D per day to meet their basic nutritional needs, including from formulations, other fortified vitamin D foods, and sources of vitamin D supplementation[4]. If food sources cannot be met, additional supplementation is recommended, especially in young children with risk factors (vitamin D deficiency in infancy, dark skin color or inadequate UV exposure, winter and spring in high northern latitudes, etc.).
(2) Calcium:
The daily milk allowance of 500 ml for young children can ensure the nutritional needs of calcium. However, some young children have obviously insufficient milk intake and need to consider the nutritional status of calcium. Children 1 to 3 years of age require 600 mg of calcium per day [17]. (3) Iron: pay attention to ensure foods rich in iron and zinc, if children have a balanced diet, they generally do not need to add other vitamins and minerals.
Have 3 main meals with your family and 2 to 3 nutritious complementary meals (fruit, milk, bread, biscuits or homemade snacks, etc.). The meal time should be 20 to 25 min / time, regular meals, children's food intake can fluctuate, do not insist on quantitative.
Eating behavior culture
Young children eat with their families, and families with conditions can let children sit in children's dining chairs to eat, which is convenient for interaction and communication with their families. Avoid watching TV or playing with toys while eating, and do not follow up on feeding. Young children should learn to grasp and use spoons, participate in the meal process, and gradually learn to eat on their own. Allow young children to eat badly and become proficient in eating techniques during eating. Cultivate children's regular eating habits, parents as far as possible to provide children with a variety of food to meet the needs of growth, do not force food. Recognizes signals that young children are full, allowing them to leave the table after eating enough. For older children, they can participate in the food making process or prepare tableware before meals to increase their interest in the eating process.
Discard bottles
At 12 months of age, learn to drink water with a straw cup, and from 15 months of age, you should abandon the bottle and drink milk or water from the cup.
Recommendations for juice intake
Infants over the age of 1 are encouraged to consume fiber-rich fruits. Even if juice is ingested, the amount should be controlled to less than 120 ml, and pure fruit juice diluted with 100% fruit juice or appropriate water should not be a beverage containing fruit juice. It is not recommended to use a bottle to consume juice, and it should be drunk in a cup.
Age at which fresh milk, honey, etc. are eaten
Because fresh milk is not fortified with nutrients, especially the supply of iron nutrition for infants, its nutrition cannot well guarantee the nutritional needs of infants under 1 year of age. Fresh milk can be ingested after the age of 1 year. As fat is still an important source of energy for young children, it is not recommended to feed low-fat or skim milk to infants and young children under 2 years of age. Honey is not recommended for infants up to 1 year of age as it is susceptible to botulinum toxin contamination [6].
Ask the children about their daily diet and nutritional balance, pay attention to the situation of picky eating, and focus on assessing eating behavior.
Growth assessment
Focus on the weight of age, the length of age, and the weight of length, and apply growth curves for nutritional evaluation [11]. Dynamically observe the growth level, rate and symmetry of young children, and find deviations and find causes in time. Children aged 1 to 2 years use their length of weight and calculate their body mass index after age 2. If the relevant measurement on the growth curve is in the 97th percentile, or the index rises or falls across the 2 major percentile curves compared with the previous assessment, it is necessary to find the cause and make timely referral if necessary.
After the age of 1 year, patients with iron deficiency in daily blood screening and poor treatment effect are referred. See guidelines for the prevention and treatment of iron deficiency and iron deficiency anaemia in children [13].
Recommendations for infant and young child feeding by age are summarized in Table 2.
(Written by Jiang Fan and Mao Meng)
Experts participating in the review and approval of this recommendation (in order of expert unit and surname pinyin): Children's Hospital Affiliated to Chongqing Medical University (Hu Yan, Li Haiqi), Hainan Provincial Maternal and Child Health Hospital (Xiang Wei), School of Public Health of Nanjing Medical University (Wang Zhiyan), Nanjing Children's Hospital affiliated to Nanjing Medical University (Li Xiaonan), Nanjing Maternal and Child Health Hospital affiliated to Nanjing Medical University (Guo Xirong), Shanghai Children's Medical Center Affiliated to Shanghai Jiao Tong University School of Medicine (Hong Li, Jiang Fan), Capital Pediatric Research Institute (Li Hui) The Second Hospital of West China Affiliated to Sichuan University (Mao Meng), the Children's Hospital Affiliated to Zhejiang University (Zhao Zhengyan)
In 2009, the Editorial Board of the Chinese Journal of Pediatrics and the Child Health Care Group of the Science Branch of the Chinese Medical Association published the "Infant and Young Child Feeding Recommendations" [1], which provided specific clinical guidance and suggestions for infant and young child feeding for child health doctors and pediatric clinicians nationwide. In recent years, with the continuous advancement of national hierarchical diagnosis and treatment, the role of grass-roots pediatric staff in children's health management has become more and more prominent. In order to adapt to the development, the Editorial Board of the Chinese Journal of Pediatrics and the Child Health Care Group of the Science Branch of the Chinese Medical Association revised the "Infant and Young Child Feeding Recommendations" [1] in 2009 with reference to the latest research progress, and wrote the "0-3 Year Old Infant Feeding Recommendations (Primary Physician Edition)" for community child health care physicians and general practitioners. This recommendation is based on children
"When it works, it spreads"
The copyright belongs to the original author, if there is any violation or infringement, please contact us