Among the many chronic diseases, dyslipidemia has become an important but difficult fortress. In China, one in about 2 elderly people has dyslipidemia; but the elderly often have the coexistence of multiple diseases and the combination of multiple drugs, and their diagnosis and treatment are unique.
Professor Ye Ping of 301 Hospital pointed out that cardiovascular disease is the main disease of death in the elderly, and > 80% of the patients who die from cardiovascular disease are the elderly. Dyslipidemia is an independent risk factor for the onset of cardiovascular disease in the elderly, and a meta-analysis[1] showed that the prevalence of dyslipidemia in the elderly in China was as high as 48%, and the prevalence of hypercholesterolemia, hypertriglyceridemia, hyperLD-Cemia, and hypoHDL-Cemia was 19.7%, 20.8%, 15.3%, and 20.2%, respectively. Why do older people become a high-incidence group of dyslipidemia? This is related to its physiological and pathological characteristics, increased absorption of LDL-C and slowed metabolism, abnormal triglycerides and HDL-C synthesis, diabetes mellitus, chronic kidney disease, thyroid dysfunction and other comorbid diseases can cause dyslipidemia.
At the same time, related studies [2] suggest that the disease awareness, treatment rate and control rate of elderly patients with dyslipidemia in China are low and need to be improved.
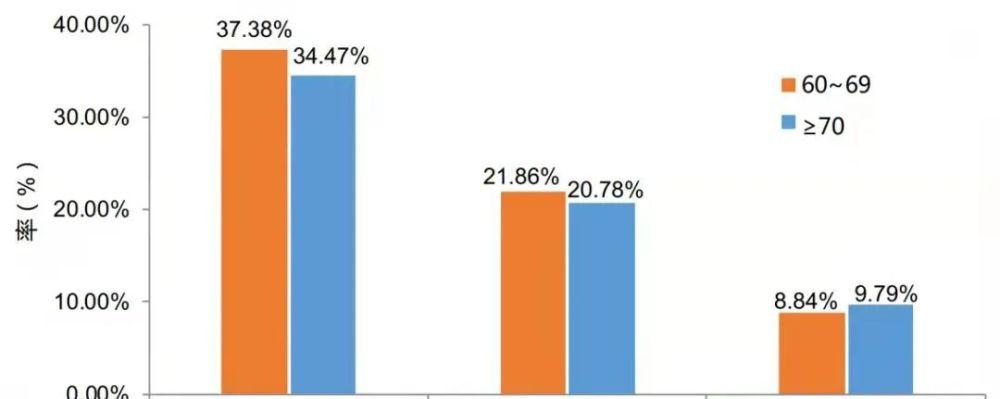
Figure 1 The disease awareness, treatment rate and control rate of elderly patients with dyslipidemia in China are low
On December 30, 2021, under the presidency of Professor Liu Meilin of the First Hospital of Peking University, the "Chinese Expert Consensus on the Management of Dyslipidemia in the Elderly" (hereinafter referred to as the Consensus) was officially released after two years of revision. As part of the Long March Project of the Chinese Society of Gerontology and Geriatrics, the revision of the consensus is aimed at standardizing the management of dyslipidemia in the elderly and promoting the prevention and treatment of atherosclerotic cardiovascular disease (ASCVD) in the elderly in China.
In this latest edition of the Consensus, it is particularly emphasized that for elderly people with dyslipidemia, lipid adjustment treatment based on individual characteristics is very important. Clinical studies have shown that statins are safe and effective in preventing atherosclerotic cardiovascular disease, and the combination therapy of the "statin +" concept is a better choice for patients who cannot lower lipids at the tolerable dose of statin or cannot tolerate treatment. In terms of the choice of options available for statin combinations, the Consensus specifically mentions that the clinical value of fish oil preparations, that is, ethyl eicosapentaenoate (IPE), is becoming more and more recognized and valued.
Blood lipid management in the elderly: emphasize the characteristics of distinguishing the population and individualized medication
Dr. Fu Zhifang of Peking University First Hospital analyzed the main contents of the Consensus from the aspects of drug treatment and integrated management strategies.
The first is the therapeutic level, where low-density lipoprotein (LDL-C) has long been the primary target for the management of dyslipidemia in the elderly. A study called DYSIS-China[3] suggested that the LDL-C compliance rate of elderly patients with dyslipidemia in China was low, with a primary prevention compliance rate of 52.4%, a secondary prevention compliance rate of 33.1%, and the compliance rate of primary hospitals was not optimistic.
Clinical evidence of statins for primary and secondary prevention in the elderly population in recent years shows that the use of statins can help reduce LDL-C levels, thereby delaying the occurrence, development and risk of cardiovascular event death in the elderly. In primary prevention of cardiovascular disease, for every 1.0 mmol/L (40 mg/dl) decrease in LDL-C, the relative risk of major vascular events was reduced by 25%, and the relative risk of major vascular events in the subgroup aged 65 to 70 years was reduced by 39%. In addition, special groups of older adults with diabetes mellitus and chronic kidney disease can also benefit from statin therapy.
In terms of safety, the consensus summarizes evidence of statins on cognitive function, stroke risk, and emerging diabetes in older patients. Multiple studies suggest that statins increase the risk of new-onset diabetes, more commonly in patients with early stages of diabetes and metabolic syndrome, and are often associated with high-dose statin use and ageing. Given that the overall benefit of statins in patients with cardiovascular disease far outweighs the risk of newly diagnosed diabetes, it is recommended that elderly patients with ASCVD take statins and monitor changes in blood glucose and glycosylated hemoglobin. When taking statins, lifestyle interventions should be intensified, followed up closely, and blood glucose abnormalities should be detected and intervened in a timely manner.
Secondly, this consensus mentions that the concept of "statin +" should be paid attention to in the field of blood lipid management in the elderly. In fact, the benefits of non-statin cholesterol-lowering drugs as well as triglycerides (fish oil preparations) in primary and secondary prevention of cardiovascular disease have been demonstrated. That is, when ASCVD or very high-risk elderly patients do not meet LDL-C standards or if triglycerides continue to rise, statins are combined with non-statins, and older patients can further benefit.
The consensus also pointed out that the formulation of elderly lipid management strategies needs to be based on the characteristics of elderly patients themselves, and a comprehensive assessment based on ascVD risk stratification, assessment of benefits and risks, and comprehensive interventions.
Maintaining a healthy lifestyle is the basic treatment measure for dyslipidemia in the elderly, and smoking cessation, alcohol restriction, reasonable diet, and regular exercise are indispensable.
drug therapy. ≤ 75-year-old patients with dyslipidemia, lipid-lowering therapy drugs are preferably statins, and whether to add or adjust drugs according to the specific conditions of the patient, and people over 75 years of age need to weigh the risks/benefits and personalize the medication.
Figure 2 Chinese expert consensus on drug selection strategies recommended by the Chinese expert consensus on the management of dyslipidemia in the elderly 2021
Most elderly people can achieve the standard with medium and small doses of statin LDL-C, so the elderly should start with small or medium doses and adjust the dose according to the efficacy when taking statins, and consider combination therapy regimens at an appropriate time. For ASCVD or very high-risk elderly patients, if triglycerides > 2.3 mmol/L after statin therapy, fibrates or fish oil preparations may be used. Lipid-regulating drugs should be used for a long time, and should not be discontinued without special reasons. After stopping the drug, blood lipids will rise or even rebound, which will significantly increase cardiovascular events and mortality.
In the era of "statin +", the concept of fish oil preparation has attracted attention
It is worth noting that the role of fish oil preparations mentioned in this Consensus in the field of blood lipid management has previously been supported by a large number of studies and literature. This field includes Research such as Reduce-IT and Evaporate, which show that high-purity EPA (fish oil preparations) can reduce blood lipid levels, and can also prevent thrombosis through anti-inflammatory, antioxidant, stable or reverse plaque, and thus prevent the occurrence of cardiovascular disease. On the other hand, fish oil health products on the market are emerging in an endless stream, but the concentration of EPA in the vast majority of products is not enough, and there may not be a conclusive benefit for cardiovascular prevention and treatment, so as to replace conventional lipid-lowering therapy may be risky.
The "fish oil preparation" recommended by the "Consensus", specifically referring to ethyl eicosapentaenoate (IPE), is currently the only high-purity (≥96%) eicosapentaenoic acid monomolecular prescription drug produced by patented technology, which is fundamentally different from ordinary fish oil health products.
In the previously released "Chinese Guidelines for the Primary Prevention of Cardiovascular Diseases 2020", there is also a related important update, that is, the recommended TG management drugs include IPE and non-norbrate, especially after the treatment of medium-dose statins in people at high risk of ASCVD, such as TG > 2.3 mmol/L, and the administration of high-dose IPE (2 g, 2 times a day) should be considered to further reduce the risk of ASCVD (recommended category II.a).
As the only IPE drug approved by the FDA to reduce the risk of cardiovascular disease in addition to TG reduction, VASCEPA has been listed in many countries in Europe and the United States. Based on the results of the Chinese clinical phase III study and other relevant global trial data, Yiteng Pharmaceutical has submitted its drug listing application in China, and expects that this innovative IPE drug can be listed in China as soon as possible, bringing more clinical benefits to middle-aged and elderly patients with cardiovascular diseases in China.
Source | A new perspective on medicine
Edit | Swagpp