There is such a complication, usually secondary to many lung diseases, such as chronic obstructive pulmonary disease, tuberculosis, pulmonary interstitial fibrosis, etc., the most common cause of which is COPD! And this complication often occurs rapidly, which can easily cause severe respiratory failure, and serious complications can also lead to abnormal heart function and endanger life!
Dr. Jin Zhe of the Department of Respiratory and Critical Care Medicine at Peking University First Hospital recently encountered such a patient.
One morning in November, at 7 o'clock, Dr. Jin Zhe of the Department of Respiratory and Critical Care Medicine of Peking University First Hospital received a WeChat message from the patient Lao Zhang: "Dr. Jin, I suddenly felt chest pain in my right side this morning, and I was still holding back badly, I sprayed emergency medicine, or it was not good, I will go to the outpatient clinic in a while, will you help me see if it is OK?" ”
Lao Zhang is a 75-year-old male patient, coughing, coughing up phlegm for more than ten years, the last 2 years of activity when shortness of breath, holding breath more and more heavy, from the initial 3 floors of feeling shortness of breath to walking on the flat ground that is, shortness of breath.
Pulmonary function test: severe hypopnea and obstructive ventilation dysfunction.
CT chest: showing emphysema in both lungs, large alveoli in the upper lobes of both lungs.
Diagnosis: chronic obstructive pulmonary disease.
Since then, Lao Zhang has followed the doctor's guidance, quit smoking, and regularly used inhalation drugs for COPD.
The drug is very effective for Lao Zhang's condition, the symptoms of coughing and coughing up sputum are not serious, and the activity endurance is also improved, and every morning after eating breakfast and inhaling the drug, he will go out to do exercise.
This morning, Lao Zhang went to the park as usual to do morning exercise, beijing winter, the weather is cold, there is a strong wind outside, Lao Zhang from the warm room to the cold outdoor, after inhaling cold air, he feels uncomfortable throat, trachea is uncomfortable, began to cough violently, and the right side of the chest sudden pain, accompanied by chest tightness, holding breath.
Lao Zhang quickly stopped his activities, slowly walked home to rest, and also used 2 sprays of vantoline (salbutamol aerosol, COPD emergency medication), but chest pain and breathing difficulties can not be alleviated, so he quickly contacted Dr. Jin Zhe and came to the outpatient clinic.
After receiving the consultation, Dr. Jin Zhe inquired about Lao Zhang's symptoms and also conducted a careful and meticulous physical examination.
Physical examination revealed that Lao Zhang's respiratory rate and pulse rate were both increased, with a respiratory rate of 30 breaths per minute, a pulse of 110 beats per minute, a blood pressure of 100 per 60 mm Hg, and a blood oxygen saturation of 85% without oxygen inhalation. Auscultation of the lungs reveals very low breath sounds in the right lung, no breath sounds in the upper middle and right lungs, and dry rales scattered in the left lung.
Patients with COPD often have emphysema, so there is often auscultation of breath sounds during lung examination, but Lao Zhang not only has a decrease and disappearance of breath sounds, but also asymmetry, which requires high suspicion of "pneumothorax".
The most important and rapid test is the "chest x-ray".
So Dr. Jin Zhe immediately arranged a chest x-ray examination for Lao Zhang, and found that the right pneumothorax was compressed by 50%. Therefore, the intravenous channel is immediately established, the nasal catheter is given oxygen, and the right thoracic cavity is continuously drained through the second intercostal puncture catheter on the lateral side of the right collarbone, which induces a large amount of bubbles.
After about 3 minutes, the patient's symptoms of holding breath and shortness of breath gradually resolve. After 2 days, there are no more bubbles overflowing in the chest cavity closed drainage bottle, and the chest x-ray is reviewed after 1 day of clamping and closing the drainage tube, and the right lung is satisfied with the recovery, so the drainage tube is pulled out and the regular inhalation drug treatment continues.
Chest pain may also be pneumothorax
Life-threatening needs to be rescued in a timely manner
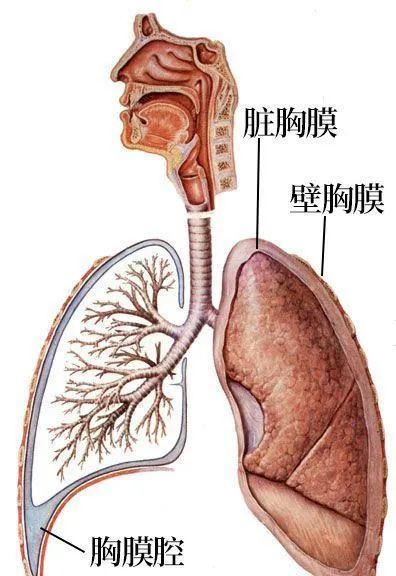
The pleural cavity is a potential space formed between the visceral pleura that covers the surface of the lungs and the parietal pleura attached to the chest wall, and normally, there is a small amount of fluid in the pleural cavity, usually 5-15 ml, which acts as lubrication during breathing. Normally, there is no gas present in the pleural cavity.
//
However, PATIENTS are often prone to complications with pneumothorax because of oxidative/antioxidant imbalances, protease/antiprotease imbalances, and chronic inflammatory effects in THE PATIENTS' airways and lung tissues.
Chronic inflammation leads to decreased elasticity at the terminal bronchiole (respiratory bronchiole, alveolar tube, alveolar sac, and alveoli), leading to increased lung volume, hyperinflation and hyperinflation of the alveoli, or accompanied by decreased lung compliance and destruction of the airway wall, which cause air to enter the alveoli but is not easily drained, which forms emphysema.
The pressure in the alveoli further increases and then the alveolar wall rupture occurs, which is fused with each other to form an air-containing cyst cavity in the lung tissue, that is, the large vesicles of the lungs, which are structures in the case of a sharp increase in pressure such as breath holding, coughing, and forceful defecation, as well as when the secretions of respiratory tract infection lead to obstruction of the small airway, the pressure in the chest cavity increases, resulting in the further stretching of the alveoli that has been expanded, and the already thinned alveolar wall may rupture and trigger the pneumothorax.
When the pneumothorax is small, the patient can have no symptoms, or only mild chest pain, which will worsen with deep inhalation, which is called pleural chest pain.
If the amount of pneumothorax is large, it will squeeze the normal lung tissue, so that the normal lung tissue can not expand with the inhalation, resulting in dyspnea, especially in patients with copernicular obstructive pulmonary and other underlying lung diseases, the reserve of lung function is less, and when the pneumothorax occurs, even if the amount is small, it may lead to symptoms such as dyspnea.
Typical symptoms of pneumothorax: chest pain, dyspnea
Dr. Jin Zhe reminds PATIENTS that because COPD itself has difficulty breathing, the clinical signs and symptoms of pneumothorax are often masked. Some patients only experience exacerbations of these symptoms on the basis of an existing cough, chest tightness, and shortness of breath. In particular, the limited pneumothorax or pulmonary compression area is small, and the examination is not easy to detect.
Therefore, when COPD patients have worsening symptoms of dyspnea, especially with chest pain, after regular treatment such as anti-infection, expansion of the bronchi, antispasmodic and asthmatic asthma, the symptoms do not improve, and even sharp aggravation occurs in a short period of time, pneumothorax should be suspected.
Graph source network
Pneumothorax requires treatment of syndromes based on specific clinical presentation, underlying disease, pneumothorax type, volume of pulmonary compression, and precipitating causes.
1. Arterial blood gas analysis can be checked, and appropriate oxygen therapy is given to patients according to the situation, usually nasal cannula oxygen.
2. When the pneumothorax volume > 15%, the patient should be punctured and pumped; when the pneumothorax volume is < 15%, if the patient's clinical symptoms are obvious and the disease progresses, the thoracentesis can also be performed.
3. When the compression of the lungs exceeds 30%, the patient should be allowed to undergo chest closed drainage as soon as possible to alleviate or prevent the development of the disease.
brief summary:
Pneumothorax is dangerous and should be dealt with in time.
Pneumothorax is often secondary to many lung diseases, such as chronic obstructive pulmonary disease, tuberculosis, pulmonary interstitial fibrosis, etc., of which the most common chronic lung disease that causes pneumothorax is COPD, and often occurs rapidly and can easily cause severe respiratory failure.
In addition, COPD patients are often older, the basic lung function is poor, when the pneumothorax volume is large, it is easy to cause mediastinum (heart) oscillation and reduction of blood volume, which in turn leads to abnormal cardiac function, which may be life-threatening in severe cases. Therefore, timely and accurate diagnosis and effective treatment of COPD complicated by pneumothorax are particularly important.
Pneumothorax secondary to COPD is prone to recurrence.
Patients with COPD pulmonary due to local lung tissue structure abnormalities, pulling capillaries, may cause vascular bed occlusion, so that the local blood supply is not good, so that the pneumothorax after the emergence of lung tissue incisus can not heal, long-term air leakage, so that most of the chest closed drainage catheter time is long, even if the healing is easy to recur. Some require surgery in thoracic surgery.
Expert Profile Jin Zhe
He graduated from Peking University School of Medicine in 2004 with a doctorate degree in clinical medicine. Since 2004, he has been working in the Department of Respiratory and Critical Care Medicine, Peking University First Hospital. Responsible for COPD and smoking cessation professional outpatient work. His main research direction is chronic obstructive pulmonary disease, and he is a member of the Beijing COPD Group.
End of this article
Please do not reprint without permission
Typography: Golden Beans