For all families looking forward to having a baby, menopause is the beginning of good news, but when they go to the examination happily, they are told that the embryo is suspended, no bleeding and no abdominal pain, how can the child be gone?! At a loss, let's take a look at ten factors that lead to embryos being stopped.
Let's start by understanding what embryos are
Embryo damage refers to the death of embryos during early pregnancy due to defects in the fertilized egg, the mother's own factors or external factors. Ultrasound findings often show withered eggs, germ without tube pulsation, and irregularly shaped germ or fetus present in the gestational sac.
Embryo abortion can be divided into two categories:
First, the fetal buds are not developed after implantation of the fertilized egg, and the color ultrasound is manifested as the fetal buds are not seen after 7 weeks of pregnancy, only an empty (fetal) sac.
The second is that there have been fetal bud development but soon stopped breeding and death, ultrasound results in the fetal sac but the development is obviously lagging behind the gestational age, while there is no fetal heart canal pulsation, the size of the fetal sac is in line with the gestational period or wilted deformation, called gestational sac wilting.
Why does embryo closure occur?
1. Anatomical abnormalities
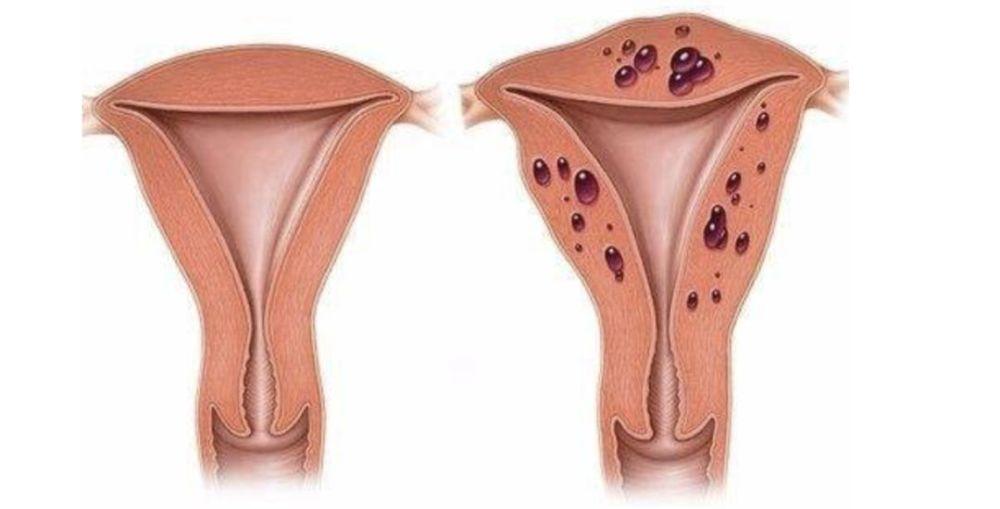
The causes of embryo arrest during early pregnancy include uterine malformations, such as uterine dysplasia, unicorn uterus, double uterus and uterine mediastinum, etc.; uterine abnormalities, such as uterine adhesions (Asherman syndrome), uterine fibroids, endometrial diseases, cervical insufficiency, etc., which can affect the intrauterine environment and uterine blood supply, thereby affecting embryo implantation and development.
2. Genetic abnormalities
The presence of abnormalities in the number or structure of chromosomes, gene polymorphisms, genetic mutations, hereditary prethrombotic states, endocrine or reproductive tract structural abnormalities, etc. in both husband and wife and embryos are genetic abnormalities.
Chromosomal abnormalities are one of the most common causes of embryos being discontinued during early pregnancy. Accounting for the gestational age
Common abnormalities in the number of chromosomes are triploids, and chromosomal structural abnormalities include chromosome deletions, overlaps, inversions, and equilibrium translocations, etc. The most common are inversion and equilibrium translocations, leading to the discontinuation of embryos in early pregnancy by chromosome 9 (p11; q13) The proportion caused by interarm inversion is higher.
Interarm inversion of chromosome 16 can also cause spontaneous miscarriage in the first trimester of pregnancy or the cessation of embryonic development. Studies have shown that the large Y karyotype has a certain genetic effect, which is related to spermatogenesis and the cessation of embryonic development in the first trimester of the spouse's pregnancy.
The large Y chromosome refers to the extension of the heterochromatin region so that the length of the Y chromosome ≥ chromosome 18, the patient's sperm has various abnormalities (azoospermia, oligospermia, dead sperm, sperm malformation), infertility, growth retardation, etc., the patient's wife can have different types of reproductive abnormalities (miscarriage, fertility genetic defect fetus, embryo stop development, stillbirth, teratology, premature birth. )
3. Infectious factors
Infectious factors that contribute to embryo cessation during early pregnancy include systemic infections and infections of the female genital tract. Chlamydia and Mycoplasma are the two most common pathogens that cause infection of the female genital tract. It can cause damage to the epithelium of the cervical mucosa, resulting in intrauterine infection, which can damage the integrity of the membrane and cause embryos to stop breeding.
Recent studies have found that bacterial or viral infections can lead to embryonic cessation, and rubella, cytomegalovirus and Toxoplasma can also cause fetal chromosomal malformations through the placenta. Other microorganisms such as Treponema pallidum, Neisseria gonorrhoeae, Listeria monocytogenes monocytogenes, and parvovirus B19, as well as rare infections such as Q fever, dengue fever, Lyme disease, and malaria, can cause embryos to stop sterilizing.
4. Immune abnormalities
Alloimmune abnormalities refer to abnormalities in the immune tolerance mechanism between mother and fetus, and the embryo is attacked by the mother's immune response to produce a rejection reaction. Fertilized eggs can be seen as a kind of semi-allogeneic transfer in the mother, and the embryo and the mother have a complex and special immune relationship, so that the mother has immune tolerance and the embryo is not rejected. Studies have shown that the number of embryonic developmental disorders is positively correlated with abnormal immune function.
The immune factors that lead to embryonic cessation are mainly in the following aspects: occlusive antibody pregnancy-related plasma protein A and other insufficient alloimmune disorders, the formation of anticardiolipin antibodies, tissue-specific antibodies, anti-sperm antibodies (AsAb), anti-endometrial antibodies (EmAb), anti-hCG antibodies and other expression enhancements. AsAb is a potent immunosuppressor in the seminal plasma that has a toxic effect on gametes and embryos by digesting macrophages, and can also directly damage trophoblast cells and cause embryonic development disorders. Tissue non-specific antibodies, antinuclear antibodies, anti-DNA antibodies, CD4+ T cell-mediated cellular immune enhancement, cell secretion of interleukin, interferon γ and tumor necrosis factor β, etc.
In addition, there is also a certain correlation between blood group incompatibility and embryonic infertility. Blood group incompatibility has ABO and Rh blood type incompatibility, and in mainland China, ABO blood type incompatibility is mainly based on the mother's O type and the fetus is A or B type. The surface of fetal erythrocytes is attached to the ABO antigen, when red blood cells enter the maternal circulation through the placenta, it can stimulate the mother to produce antibodies, causing the same immune response caused by maternal-fetal blood group incompatibility, directly affecting embryonic development and causing miscarriage.
5. Endocrine abnormalities
Luteal insufficiency (LPD), elevated prolactin (PRL), polycystic ovary syndrome (PCOS), thyroid disease, etc. are important endocrine factors that cause embryonic infertility, which can affect the function of the hypothalamic-pituitary-ovarian axis, mainly manifested as abnormal secretion of progesterone and its metabolites, resulting in early miscarriage.
Luteal insufficiency is due to insufficient production of progesterone or short maintenance time of the luteum, endometrial dysplasia or endometrial maturation delay of more than 2 days, hindering the implantation of pregnant eggs and embryonic development and causing miscarriage, clinical generally need to increase the progesterone content in the body by oral progesterone capsules or intramuscular HCG and progesterone injections to achieve fetal preservation effect.
Patients with polycystic ovary syndrome, treated with metformin during pregnancy, have a significantly reduced miscarriage rate.
Abnormal pituitary gland function or mass lesions can cause hyperprolactinemia, inhibit hypothalamic gonadotropin synthesis and release, cause follicle development and ovulation disorders, and interfere with fertilization and embryonic development, resulting in embryonic cessation.
There is still controversy about whether bromocriptine is discontinued after pregnancy in patients with hyperprolactinemia. For patients with prolactin microadenoma after pregnancy, if bromocriptine is discontinued, it should be re-examined every 2 months, and bromocriptine treatment should be restarted if headache or visual impairment occurs.
Patients with thyroid dysfunction, such as hypothyroidism, use thyroxine or levothyroxine sodium, while those with hyperthyroidism should be pregnant after hyperthyroidism is controlled, and the changes in the condition should be closely observed during pregnancy.
6. Prethrombotic state - thrombosis
Also known as hypercoagulable blood, refers to a state in which the concentration of coagulation factors is increased, or the concentration of coagulation inhibitors is reduced, the blood is easily coagulated, and it has not yet reached the level of thrombosis, or a small number of thrombuses formed are in a dissolved state. At present, the antiphospholipid antibody syndrome is more studied, and it has been confirmed that it is associated with early and middle fetal loss.
The general view is that hypercoagulable state changes the blood flow status of the placenta of the uterus, easy to form local microthrombosis, and even placental infarction, so that the placental blood supply decreases, embryonic or fetal ischemia and hypoxia, causing embryonic or fetal dysplasia and miscarriage.
Low molecular weight heparin (LMWH) alone or in combination with aspirin is currently the mainstay of treatment. The general dosage of low molecular weight heparin is 5000U subcutaneously, 2 times a day. The duration of the medication begins in the early trimester. For patients of a heavier degree or who have not used aspirin before pregnancy, the drug should be started before ovulation. Reports indicate that the clinical effect of aspirin alone is not as good as that of low molecular weight heparin alone or a combination of both.
7. Environmental factors
With the advancement of society and science and technology, environmental factors have received more and more attention on the impact of embryo cessation in early pregnancy. Environmental influences can impair or interfere with reproductive function, leading to embryos being suspended. The environmental factors that were previously believed to lead to embryo cessation during early pregnancy mainly include three categories:
Physical factors: X-rays, microwaves, noise, ultrasound and high temperatures.
Chemical factors: chemical drugs and ionizing radiation, etc.
Bad lifestyle habits: alcoholism, smoking, drugs and coffee.
8. Psychological factors
Emotional tension puts the body in a state of stress, destroys the original stable state, and causes neuroimmunity and endocrine disorders in the body, especially the change of progesterone. The level of progesterone in the body decreases, and the embryo is stunted, resulting in fetal cessation. Therefore, pregnant women should pay attention to adjusting their emotions and avoid excessive mental tension.
9. Traumatic stimulation
Uterine trauma such as surgery, direct impact, and overcourse can also lead to fetal arrest.
10. The embryo stops developing for unknown reasons
Studies have found that vascular insufficiency and apoptosis during placental formation are one of the important factors that lead to embryonic stop development. Abnormal expression of deciduous angiogenesis and angiogenic factors such as VEGF, placental growth factor, angiogenesis, matrix metalloproteinases, Notch receptor proteins, etc., through a series of cascading reactions, participate in the occurrence of blood vessels, affect the nutrition of the placenta to the embryo, resulting in the cessation of embryonic development.