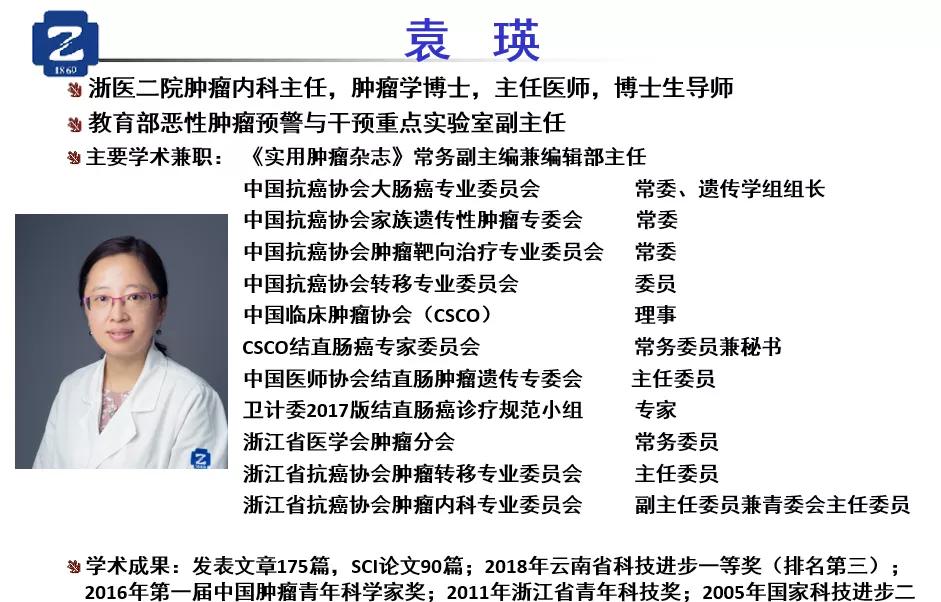
Author/Second Affiliated Hospital of Zhejiang University School of Medicine Yuan Ying Hu Hanguang Zhong Chenhan
disgust The 2020 ASCO conference came to an end, and this year the colorectal cancer field has gained a lot in the field of perioperative and advanced palliative care. The immunotherapy related content is summarized, including patients with msi-h and mss, and some key studies that may be helpful in clinical practice are selected to share with you.
The brightest study in the field of colorectal cancer this year spent on immunotherapy, the Keynote-177 study. Previous research data tell us that patients with MSI-H are the most beneficial group of people from immunotherapy, and the CSCO guidelines recommend the treatment of PD-1 for palliative second-line and above treatment in patients with MSI-H. However, in palliative first-line therapy, should msi-h patients be treated with pd-1 immediately, or should they be treated with conventional chemotherapy in combination with targeted therapy? keynote-177 is here to answer this question.
【lba4:keynote-177(immune msi-h)】
Keynote-177 targeted patients with newly treated advanced MSI-h colorectal cancer in two groups, one using a single-agent pembolizumab (200 mg every 3 weeks) and the other using a chemotherapy ± targeted regimen that follows the guidelines selected by doctors, of which 18.9% of patients were given folfox or folfiri with two-drug chemotherapy alone. In addition, the study allowed first-line chemotherapy ± crossover to the pambolizumab group after targeted therapy progression, 36% of patients in the study crossed to pambolizumab, plus 36 patients who used pambolizumab outside the study, so overall 59% of patients used pd-1 after chemotherapy ± targeted therapy progression. The primary endpoint of this study was progression-free survival (PFS).
The results showed that the difference between the two groups of PFS was very obvious, the PFS of the chemotherapy ± targeted therapy group was 8.2 months, and the PFS of the pambolizumab monotherapy group was 16.5 months, which doubled the increase. From the overall effective rate (orr) data, the effective rate of chemotherapy ± targeted therapy group was 33.1%, and the effective rate of the pambolizumab monotherapy group was 43.8%. From the perspective of adverse reactions, adverse reactions of 3 degrees and above, chemotherapy ± targeted therapy group was 66%, and pambolizumab monotherapy group was 22%
Therefore, the results from the keynote-177 study showed that for MSI-H patients with primary MCRC, immunotherapy PD-1 beat conventional chemotherapy ± targeted therapy.
【4040:checkmate-142(immune msi-h)】
The checkmate-142 study is a multi-cohort study of patients with msi-h around nivolumab. One of the cohorts was the use of nivolumab monoclonal antibody (3 mg/kg every 2 weeks) plus low-dose ipilimumab (1 mg/kg every 6 weeks) in advanced first-line therapy, and the results of the long-term follow-up were updated at this asco meeting. Although the entire cohort included only 45 patients, the orr reached 69% and the 2-year PFS reached 74%.
Both keynote-177 and checkmate-142 studies were studies of late first-line treatment in MSI-h patients using immunotherapy.
We compared the data from the two studies horizontally to get four clinical implications:
1. In MSI-h patients, advanced first-line chemotherapy ± targeted therapy will be replaced by immune checkpoint inhibitors, and domestic and foreign guidelines will be rewritten.
2, research suggests that MSI-h patients are a special group of patients, their treatment will be completely different from other patients, the treatment of immune checkpoint inhibitors for these patients opened a new treatment path, chemo-free may become a reality. The detection of MSI should be given more attention, and the initial diagnosis should be clear.
3. The chemotherapy ± first-line treatment PFS in the keynote-177 study was only 8.2 months, orr was only 33.1%, which was worse than the efficacy of conventional first-line treatment in the general population, suggesting that MSI-h patients were less likely to be effective ± conventional chemotherapy than MSS patients.
4. Horizontal comparison of keynote-177 and checkmate-142 research data suggests that the combination of double exemption may be more effective than single exemption treatment.
Because in clinical practice, only about 5% of MCC patients have the MSI-h phenotype, while the vast majority of patients are mss. So, then we turn our attention to immunotherapy for patients with colorectal cancer. It is already an indisputable fact that monotherapy immune checkpoint inhibitors are ineffective in mss patients.
How to break through the efficacy of these patients is the direction that has been working hard for all these years. The 2019 ASCO conference reported that the reconvio study, that is, the combination of navumab and rigofenib in patients with MCCs who had failed to follow the standard treatment, still achieved a 33% effective rate in 25 patients with MCCs, which received widespread attention for a time.
In this year's ASCO, we can still see a lot of exploratory studies, combined with immune checkpoint inhibitors and other drugs, hoping to make a breakthrough for MSS patients. Among them, 3006 is a palliative first-line treatment study, and the others are all back-line treatment studies.
【3006:folfox + devalumab + ctla4 (immune MSS)】
This study is an exploratory study of the ib/ii phase. First-line treatment for patients with MSS MCRC is treated with traditional folfox chemotherapy combined with pd-L1 inhibitors (devaluzumab) and ctla4 inhibitors (tremelimumab), i.e., dual immunotherapy. In this study, folfox was used for 6 cycles; devaluzumab was given every 2 weeks until tumor progression or toxic intolerance; tremelimumab was used every 4 weeks for a total of 4 doses. The study included only 16 patients, but the results were encouraging. In the FOLFOX+PD-L1+CTLA-4 group, ORR 62% and DCR87.5%, of which 25% of patients achieved complete remission (CR).
Next, we will briefly share the results of the study of three anti-vascular small molecule tki drugs combined with PD-1/PD-L1 inhibitors in the treatment of advanced bowel cancer.
[4019: Regomune study (reg+ave) (immune MSS)]
This was a single-arm phase II study of non-MSI-h patients using regofenib (160 mg QD, discontinued for 3 weeks) plus a PD-L1 inhibitor (avelumab, 10 mg/kg every 2 weeks). A total of 48 patients were enrolled in this study, all of whom failed standard treatment. Efficacy of 40 patients could be evaluated: 23 patients (57.5%) with stable disease (sd), including 12 cases (30%) with reduced tumor burden; 17 cases (42.5%) with disease progression (pd); median pfs at 3.6 months and median os at 10.8 months, the results should be said to be unsatisfactory.
【4028: Furuquintinib + sindilimab (immune)】
This was a study from China in which a total of 52 patients with re-treatment mcC were treated with furuquintinib (3 mg, discontinued for 3 weeks) + sindilimab (200 mg q3w). The main findings were: orr: 15.38% (8/52), dcr: 57.6% (30/52), and median pfs at 108 days.
【4031:mek inhibitor + bevac + pabrilizumab (immune)】
This is a clinical study of patients with MSS MCRC who have failed standard therapy, using the MEK inhibitor binimetinib (45 mg po bid) in combination with perorizumab (200 mg iv q3w) and bevacizumab (7.5 mg/kg iv q3w) in a Phase II single-arm study. The primary endpoints were safety, tolerance, and orr. The 21 patients reported were all mss-type, including 10 kras/nras mutations and 11 ras wild-type patients. Efficacy in 17 patients: PR 2 (12%), SD 14 (82%), DCR 16 (94%), 1 case with pd.
From the two studies of keynote-177 and checkmate-142, it can be seen that palliative first-line therapy in MSI-h patients is superior to single-agent pd-1 is superior to chemotherapy ± targeted therapy recommended by current guidelines, and double-immune therapy may be better.
For MSS patients, there has been no big breakthrough this year. However, although the number of cases of folfox + devaluzumab + ctla4 treatment in palliative first-line treatment is very small, the prospect of first-line treatment is still good; the mek inhibitor + bevacizumab + pabolizumab of post-line treatment is also worth looking forward to. If there can be a larger sample size accumulation and validation in the follow-up, then an immunotherapy breakthrough in MSS patients is not a dream.
#医师报超能团 #
#超能健康团 #
#健康科普排位赛 #