The endometrium is closely related to women's health, so the "thickness of the endometrium" on the B ultrasound checklist always affects the heartstrings of countless women.
Often, the girl will ask the doctor with an anxious face:
"My uterine lining is thin, can I get pregnant?"
Today, Zhimei will talk about this problem.
Under normal circumstances, the endometrium is like a leek growing from stubble, which changes with the menstrual cycle, first proliferating, then falling off and discharging, which is menstrual blood [1].
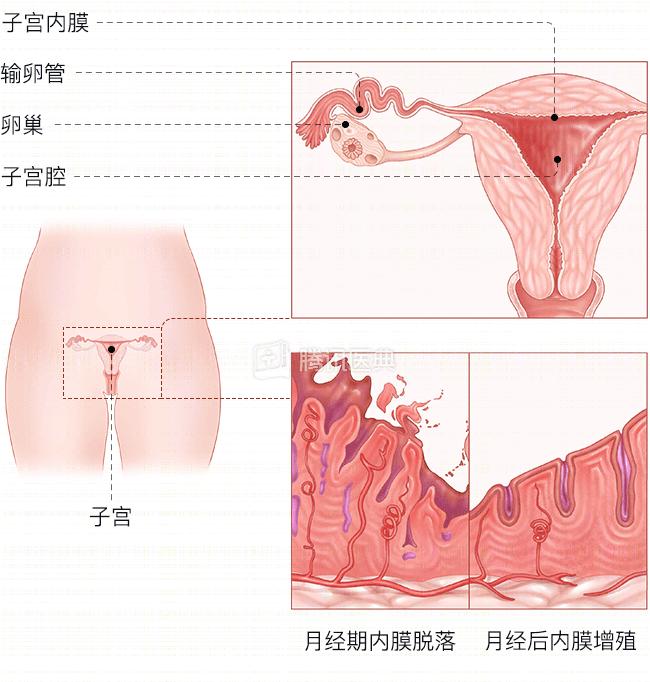
To subdivide it, the endometrium can be divided into functional layers and basal layers, which are like the branches and rhizomes of leeks.
"Branches and leaves" (functional layers) under the action of estrogen and progesterone, will undergo periodic changes, continuous growth - shedding;
The "rhizome" (the base layer) is like a logistics personnel, transporting "supplies", repairing wounds, and letting the functional layer "spring breeze blow and grow again".
Therefore, the thickness of the endometrium varies with the menstrual cycle.
On days 5 to 14 of the menstrual cycle (proliferative period), the endometrial thickness gradually thickens to 5 to 11 mm [2].
(Source: Nemours KidsHealth)
By the 15th to 28th day of the menstrual cycle (secretory phase), the endometrium continues to thicken, gradually becoming thicker and softer.
Like a layer of fertile soil, it becomes suitable for the implantation and development of new life, reaching a thickness of about 16 mm [2].
Therefore, if you do B ultrasound at the end of menstruation, at this time the intima has just grown up, it is normal to be thin, and there is no problem.
Although there have been clinical and case reports of successful pregnancies of endometrium of 5 mm or even 4 mm, large sample studies have shown endometrial thickness [3,4].
Currently, most studies suggest that the endometrium is <7 mm thick on day 14 of ovulation, which can be called a thin endometrium [5].
An overly thin endometrium is often accompanied by poor endometrial glands and angiogenesis, like not enough fertile soil, making it difficult for the embryo to implant.
Furthermore, the thin endometrium may also hinder the invasion of the trophoblast layer (the outermost layer of the blastocyst, most of which develops into a placenta), increasing the risk of early miscarriage [3].
(Source: Wikipedia contributors)
Therefore, if the sister has too little menstruation (menstrual days < 3 days, menstrual blood volume <5 ml), it is recommended to go to the gynecology department in time [6,7].
If you are not sure about your menstrual volume, you can start with a simple assessment at home using the graphed menstruation method (SAP-c version).
The thicker the uterine lining, the better.
In general, ultrasound B is done when menstruation is just clean (days 6 to 14 of the menstrual cycle), and the thickness of the endometrium should be between 5 mm and 7 mm [2].
If the endometrium is thicker than normal, and there is non-menstrual bleeding or post-intercourse bleeding, large menstrual flow or accompanied by symptoms such as blood clots, prolonged menstruation, and incomplete dripping, it is recommended to consult a gynecologist in a timely manner [8].
If the menstruation is normal, you can rest assured, you can wait for the next 1 or 2 days after the menstrual clean, the lining is clean and returned to a normal state, and then go back to the review.
In addition, there are some women to pay special attention to, that is, postmenopausal women.
After menopause, the endometrium should thin if there is no estrogen supplementation.
If the thickness of the endometrium is found to be more than 5 mm at this time [9,10], it is recommended to go to the gynecology department in time to rule out malignant lesions of the endometrium, especially in women with vaginal bleeding after menopause.
Reviewer
Liu Haiphong | Deputy Chief Physician of the Department of Obstetrics and Gynecology, Huashan Hospital, Fudan University
bibliography
[1] Dasharathy SS, Mumford SL, Pollack AZ, et al. Menstrual bleeding patterns among regularly menstruating women. Am J Epidemiol. 2012;175(6):536-545. doi:10.1093/aje/kwr356
[2] Nalaboff KM, Pellerito JS, Ben-Levi E. Imaging the endometrium: disease and normalvariants. Radiographics.2001;21(6):1409-1424.doi:10.1148/radiographics.21.6.g01nv211409
[3] Mahajan N, Sharma S: The endometrium in assisted reproductive technology: How thin is thin? J Hum Reprod Sci 2016, 9(1):3-8.
Ding Zhaofei, Tian Li. A study on the threshold method for the diagnosis of thin endometrium[J].Chinese Clinical Journal of Obstetrics and Gynecology, 2018, 19(4): 291-294. DOI: 10.13390/j.
[5] Zhao J, Zhang Q, Li Y: The effect of endometrial thickness and pattern measured by ultrasonography on pregnancy outcomes during IVF-ET cycles. Reprod Biol Endocrinol 2012, 10:100.
[6] Wouk N, Helton M. Abnormal Uterine Bleeding in Premenopausal Women. Am Fam Physician. 2019 Apr 1;99(7):435-443. PMID: 30932448.
Gynecology Endocrinology Group, Obstetrics and Gynecology Branch of Chinese Medical Association. Guidelines for the diagnosis and treatment of abnormal uterine bleeding[J]. Chin J Obstetrics and Gynecology,2014,49(11):801-806.DOI: 10.3760/cma.j.issn.0529-567x.2014.11.001.
[8] Saso S, Chatterjee J, Georgiou E, Ditri A M, Smith J R, Ghaem-Maghami S et al. Endometrial cancer BMJ 2011; 343 :d3954 doi:10.1136/bmj.d3954
[9] Goldstein SR. The role of transvaginal ultrasound or endometrial biopsy in the evaluation of the menopausal endometrium. Am J Obstet Gynecol. 2009 Jul;201(1):5-11. doi: 10.1016/j.ajog.2009.02.006. PMID: 19576369.
[10] Saarelainen SK, Vuento MH, Kirkinen P, M enp JU. Preoperative assessment of endometrial carcinoma by three-dimensional power Doppler angiography. Ultrasound Obstet Gynecol. 2012 Apr;39(4):466-72. doi: 10.1002/uog.10103. Epub 2012 Mar 12. PMID: 21953858.
Content production