This article is reproduced from: Medical Community Cardiac Endocrinology Channel
This article is written by Lü Xiong
This article is reviewed: Wang Jianhua, director of the Diabetes Diagnosis and Treatment Center of Jinan Hospital in Shandong Province
Diabetes mellitus is a group of metabolic diseases characterized by high blood sugar. Hyperglycemia is caused by a defect in insulin secretion or impaired biological action, or both. Long-standing hyperglycemia leads to chronic damage and dysfunction of various tissues, especially the eyes, kidneys, heart, blood vessels, and nerves. Diabetes indicators are important reference bases for the diagnosis of diseases, the judgment of diseases, and the formulation of individualized treatment plans.
Factors influencing blood glucose detection
Before we can understand the various test indicators, we must first know that collecting blood that meets the requirements is key. The capillary blood glucose of the household blood glucose meter is generally used as a daily blood glucose monitoring for diabetic patients and cannot be used for the diagnosis of diabetes, which requires the detection of glucose content in venous plasma (or serum).
Long-term nervousness and anxiety, insomnia before blood draw, some diseases or stress states such as colds, inflammation, acute infections, trauma, etc., may lead to high fasting blood glucose and the formation of transient "stress hyperglycemia". Before measuring blood glucose, we must rule out such situations, so that the test results can truly reflect their own blood glucose levels;
Some drugs, such as vitamin C, can have an impact on blood glucose test results. Vitamin C is a reducing agent, which may chemically react with the reagents for blood glucose and urine glucose, so that the blood glucose and urine glucose results of the laboratory test are biased, so we must consider the impact of drugs before measuring blood glucose.
Standard Oral Glucose Tolerance Test (OGTT)
The standard oral glucose tolerance test can obtain the values of fasting blood glucose and postprandial blood glucose to understand the function of islet β cells and the body's ability to regulate blood sugar, which is a confirmatory test for diagnosing diabetes and is widely used in clinical practice.
Detection method: Overnight fasting 8 to 10 hours later, in the morning before 8 o'clock in the morning to draw venous blood, you can obtain fasting blood glucose value; and then oral oral 75 grams of anhydrous glucose plus 250 ml ~ 300 ml of water made of aqueous solution, from the first sip of timekeeping, respectively, 30 min, 60 min, 2 h, 3 h and other time points of blood glucose values, and fasting blood glucose values composed of 5 time points of blood glucose values for testing.
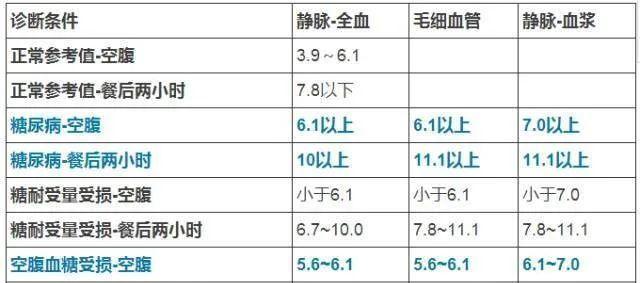
Table 1 Corresponding normal range values of OGTT detection (units are mmol/L)
Glycosylated hemoglobin (HbA1c)
The 2020 edition of the China Guidelines for the Prevention and Treatment of Type 2 Diabetes uses HbA1c measured under standardized methods as a supplementary diagnostic criterion for diabetes. HbA1c is HbA1c formed by the slow and irreversible non-enzymatic reaction of some special molecular parts of hemoglobin and glucose, which can reflect the average blood glucose level in the last 8 to 12 weeks, and is a common criterion for judging blood glucose control in diabetic patients. The normal reference value for HbA1c is 4% to 6%.
It should be noted that HbA1c reflects the average level of blood glucose control in recent times, and does not reflect the fluctuation of blood glucose, normal HbA1c does not mean that there is no problem with blood sugar, anemia, hemoglobin abnormalities and other factors may affect the accuracy of the results.
Time within the target range
(Time in Range,TIR)
According to the TIR International Consensus Recommendation, TIR refers to the time (min) or percentage (%) of diabetics in the target range (usually 3.9 to 10.0 mmol/L) within 24 hours of the day. Diabetic patients are usually required to control blood glucose between 3.9 and 10mmol/L in more than 70% of the time in 24 hours a day, which is considered to be a blood glucose control standard, but should be highly individualized, while paying attention to hypoglycemia and blood glucose fluctuations.
The significance of TIR is to understand the protection and regulation of blood glucose homeostasis, which can more accurately prevent patients from developing various diabetic complications and effectively control the progression of the disease. The commonly used blood glucose evaluation indicators in the clinic include blood glucose and HbA1c, which have certain limitations, and it is impossible to describe whether the patient's daily blood glucose fluctuations are in the normal range, one is too microscopic, one is too macroscopic.
The organic combination of blood glucose, HbA1c and TIR is an ideal blood glucose monitoring mode, which can more comprehensively reflect the true situation of patient blood glucose control and provide sufficient decision-making basis for refined adjustment of treatment plans.
Glycoprotein (GA)
GA is the product of a non-enzymatic reaction of serum proteins (mainly albumin) with glucose, because the albumin half-life is 17 to 20 days, and GA reflects the average blood glucose in the 2 to 3 weeks before the measurement. GA is quantitatively determined on the basis of GSP (glycosylated serum protein), using the percentage of serum GA to serum albumin to indicate the level of GA, removing the effect of serum albumin level on the test results, so it is more accurate than GSP.
The reference range of GA normal values is 11% to 17%. Compared with HbA1c, GA is more sensitive to short-term blood glucose changes than HbA1c, which is a good indicator for evaluating the short-term glucose metabolism control of patients, especially for diabetic patients with adjusted treatment regimens. In addition, for diabetic patients with factors that affect the longevity of red blood cells, HbA1c numerical measurement is often underestimated, then it is suitable to choose GA, the value is not affected, GA is more reflective of blood glucose control than HbA1c.
Urine sugar
Urine glucose refers to the sugars in the urine, mainly the glucose in the urine. Normal people have very little urine sugar, and the general method cannot detect it, so normal people should have negative urine glucose, or there should be no sugar in the urine. Only when the blood sugar exceeds 160 to 180 mg/dl, the sugar can be more excreted from the urine to form urine sugar.
Under normal circumstances, the kidneys' glomeruli have a strong reabsorption capacity for glucose, but this ability is limited, when the blood glucose concentration exceeds the kidney glucose threshold (generally 8.9 to 10.0 mmol/L), glucose will be excreted with the urine, showing positive urine glucose, which can indirectly reflect blood glucose levels. In general, there is an empirical correspondence between "urine sugar +" and "blood sugar" as follows:
Table 2 Correspondence between "urine sugar +" and "blood glucose"
Note: Positive urine glucose is not used to diagnose diabetes. Whether there is a "+" in urine glucose is related to blood glucose concentration, whether the renal glucose threshold is raised or decreased, stress factors and other diseases, which can be divided into "glycemic increased diabetes", "blood glucose normal diabetes", "transient diabetes" and "disease-related diabetes".
Urinary ketones
Urinary ketones are a general term for three different components, which are acetone, acetoacetic acid, and β-hydroxybutyric acid, which are intermediate products of fat metabolism in the body. In general, it is produced very rarely, and the normal human ketone body qualitative test is negative. In hunger, various reasons caused by the occurrence of sugar metabolism disorders of lipid breakdown increased and diabetic acidosis, because the rate of production of ketone body is greater than the rate of tissue utilization, ketoemia can occur, followed by ketonuria, then the situation is not optimistic, should go to the hospital in time to avoid unnecessary injury.
Severe diabetic patients due to severe lack of insulin in the body caused by the body can not metabolize sugars to provide energy for the body, the body in order to maintain normal physiological functions will consume fat and produce a large number of ketone body in the blood accumulation, causing diabetic ketoacidosis, urine ketone body 2 "+" or more can be used as a reference diagnostic standard for ketoacidosis.
Insulin autoantibodies
There are two cases of insulin antibodies, one occurs in patients receiving exogenous insulin therapy, mainly related to the purity of insulin preparations, and the other occurs in patients who have never received insulin therapy, called insulin autoantibodies. Insulin antibodies are of great significance for the diagnosis, differential diagnosis and treatment of diabetes mellitus and hypoglycemia.
Early detection of type 1 diabetes: Normal people who find insulin antibodies in the blood may develop type 1 diabetes. Detection of insulin autoantibodies can be used as a marker of autoimmune islet cell damage and can be used for early detection and prevention of type 1 diabetes.
Diagnosis of insulin resistance, guidance of diabetes treatment: the presence of insulin antibodies in the blood is an important cause of insulin resistance, diabetics can be insulin resistance due to the production of insulin antibodies in the process of using insulin therapy, manifested by increasing insulin dosage day by day but blood glucose control is not ideal. Insulin antibodies should be measured at this time, and positive or elevated titers can be used as an objective basis for insulin resistance.