Lipoprotein-associated phospholipase A2 (Lp-PLA2), also known as platelet activating factor acephthalein hydrolase (PAF-AH), is a phospholipase secreted by inflammatory cells that can promote the hydrolysis of phospholipids, which is a member of the phospholipase superfamily of phospholipase A2 (PLA2), with a relative molecular mass of 45. 4 kD (441 amino acids).
First, the function of Lp-PLA2
The basic function of Lp-PLA2 is to catalyze the hydrolysis of vinegar bonds on various oxidized phospholipids Sn-2 positions to produce free arithypic acid and hemolytic phospholipids. In addition, Lp-PLA2 can hydrolyze inflammatory factors such as platelet activators.
Second, the biological characteristics of Lp-PLA2
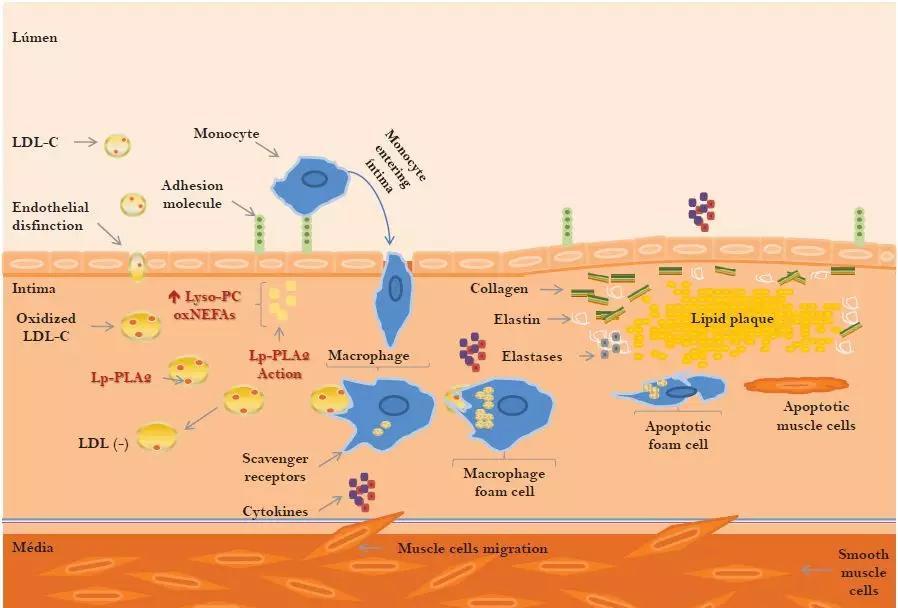
Lp-PLA2 is a subtype of the phospholipase superfamily, also known as platelet activating factor acetyl hydrolase, which is secreted by macrophages, T cells, and mast cells in the lining of blood vessels. Lp-PLA2 expression is upregulated in atherosclerotic plaques and strongly expressed in macrophages with fibrous caps of vulnerable plaques. Lp-PLA2 hydrolyzed oxidation Phospholipids in LDL produce lipid pro-inflammatory substances such as hemolytic lecithin and oxidative free fatty acids, which in turn produce a variety of atherosclerotic effects, including endothelial cell death and abnormal endothelial function, stimulating the production of adhesion factors and cytokines. These substances can further produce self-reinforcing cycles by chemotaxis inflammatory cells, producing more pro-inflammatory substances.
Lp-PLA2 released into the blood circulation binds mainly to lipoproteins rich in apolipoprotein (Apo)B, with low-density lipoprotein (LDL) accounting for 80%, and the rest binding to high-density lipoprotein (HDL), lipoprotein, and very low-density lipoprotein (VLDL). In patients with atherosclerotic disease, Lp-PLA2 levels were positively correlated with LDL subcomponent levels.
Third, the clinical detection of Lp-PLA2
There are two kinds of detection of Lp-PLA2: active method and concentration method. The active method mainly adopts high performance liquid chromatography, radioactivity determination and enzyme hydrolysis substrate method. HPLC has low sensitivity and is susceptible to interference from various components in the blood. The radioactivity measurement method has problems such as radioactive contamination, low accuracy and poor repeatability of reagents; the enzyme hydrolysis substrate method mainly relies on imported reagents, and there are problems of high cost. In the clinic, the method of detecting concentration is mainly elisa method. The EUSA method uses solid-phase sandwich method test, and the standard with known Lp-PLA2 concentration and the sample with unknown concentration are added to the microplate plate for detection. Lp-PLA2 and biotin-labeled antibodies are incubated simultaneously. After washing, add the affinity-labeled HRP. After incubation and washing, the unbound enzyme conjugates are removed, and then substrates A and B are added, and the enzyme conjugates act simultaneously. Produces color. The shade of color is positively correlated with the concentration of Lp-PLA in the sample.
Lipoprotein phospholipase a2 is a substance that marks inflammation.
In recent years, the incidence of cardiovascular and cerebrovascular diseases has become higher and higher, and in order to prevent and solve such diseases, many studies have been done in medicine and many ways have been developed to check the causative factors. Lipoprotein phosphatidase, as the name suggests, is composed of fat protein phospholipids. Therefore, the marker is not harmful to the human body. It was also a great discovery in medicine. So what exactly is lipoprotein phospholipase a2?
(1) Atherosclerotic cardiovascular disease is the primary cause of death and disability. In addition to dyslipidemia, inflammation and oxidative stress are also important mechanisms for the pathophysiology and development of atherosclerosis. At present, domestic and foreign guidelines recommend the use of traditional risk factor-based models to predict the short- and long-term risk of atherosclerotic cardiovascular disease. However, there are still deficiencies in the use of traditional risk factors alone, such as differences in the risk of cardiovascular disease events in individuals with the same risk factors, cardiovascular disease events in some patients who do not have traditional risk factors, and residual risk in patients receiving adequate statin therapy. Biomarkers are considered an important complement to traditional risk assessments. Unlike C-reactive protein (CRP), lipoprotein-associated phospholipase A2 (Lp-PLA2) is a vascular-specific marker of inflammation, and Lp-PLA2 has been found to be an independent risk factor for coronary heart disease and ischemic stroke. It was recently approved by the U.S. FDA for the prediction of coronary heart disease and ischemic stroke risk.
(2) Lp-PLA2 released into the blood circulation is mainly bound to lipoprotein rich in apolipoprotein (Apo)B, low-density lipoprotein (LDL) accounts for 80%, and the rest binds to high-density lipoprotein (HDL), lipoprotein a [Lp(a)] and very low-density lipoprotein (VLDL). In patients with atherosclerotic disease, Lp-PLA2 levels were positively correlated with LDL subcomponent levels.
(3) Lp-PLA2 levels can be reflected by measuring serum (plasma) Lp-PLA2 activity and quality, and it is clinically recommended to determine the quality of serum Lp-PLA2, and there are commercial kits available for clinical testing. Mainly using luminescent immunoassay and enzyme-linked immunosorbent assay (ELISA), the former above the forwarding light immunoassay as a representative, with simple operation, stable results, good repeatability and other characteristics; the latter is represented by PLAC method, the operation is slightly complex, there are many influencing factors, but as a high-throughput detection, it can meet the needs of large sample detection.
(4) Lp-PLA2 is affected by small physiological variations, basically not affected by receptor position changes and daily activities, so there is no need to fix the position and time when collecting specimens, no need for fasting, but strenuous exercise should be avoided 2h before measurement. [5] Lp-PLA2 test samples can be measured with dipotassium EDTA-K2, heparin anticoagulant plasma, sodium citrate anticoagulant plasma, and serum. As soon as possible after blood draw, the plasma (clear) is isolated and measured in time, the specimen can be stored for 1 week at 2-8 °C, -20 °C can be stored for 3 months, and -70 °C can be stored for a longer time (it is best to use serum, which can be stably stored for more than 5 years).
Conclusion: The reference value of lipoprotein-associated phospholipase A2 is 0-175, which may vary in different hospitals, and if plasma lipoprotein phospholipase a2 is slightly higher, it generally indicates that this cardiovascular and cerebrovascular and thrombotic arteriosclerosclerosis disease is a predictive target, but not a clinical diagnostic target. It is recommended that cardiovascular and cerebrovascular diseases should be prevented, the diet should be light, low fat, low salt, appropriate exercise, such as walking, jogging, etc., and go to the hospital for examination and treatment in time.