Have you found that no matter when and where you go to the reproductive clinic, the doctor will often say, "Draw a blood, check the endocrine hormone."
As a patient, every time you hold the test sheet, look at the same value every time, confused, and the doctor can decipher the information according to the hormone "code", so as to grasp the patient's physical condition.
So how are these unpredictable hormones analyzed? Let's knead and knead and talk about the six endocrine items.
What do the six sex hormones represent?
Members of this "female group" of reproductive hormones: follicle-stimulating hormone (FSH), luteinizing hormone (LH), prolactin (PRL), estradiol (E2), progesterone (P), testosterone (T).
- 1 -
Follicle-stimulating hormone (FSH), luteinizing hormone (LH)
Their origins let's start with the fact that FSH and LH are glycoprotein hormones secreted by the pituitary gland, and their role, as the name suggests, follicle stimulating hormone (FSH) is a key hormone that stimulates follicle growth, is the "power" source of follicle development, and is "eating" hormones to grow up. Luteinizing hormone (LH), on the other hand, tends to exert force in the second half of the process to promote the final maturation of the follicle, help the egg break through the siege, break free of the shackles in the ovaries, and induce the completion of ovulation.
- 2 -
Prolactin (PRL)
Prolactin (PRL) is a protein hormone synthesized by the pituitary gland, and it is also a hormone that sees the essence (action) through the name, and is in a normal non-pregnant state with low levels. Once the pregnancy and lactation period are further increased, the role is to promote the growth and development of the breast glands and the formation and secretion of milk.
For PRL, it has its own "personality", rhythm fluctuations throughout the day, resulting in its highest at nighttime sleep, the lowest at 9-11 o'clock during the day, in line with the principle of "low is not high", we will recommend patients to do this test in the morning. It should be pointed out that there are many interfering factors that affect the rise of prolactin, and the general PRL is within 3 times of the normal range, and it is recommended to recheck again, so there is no need to blindly nervous about mild elevation.
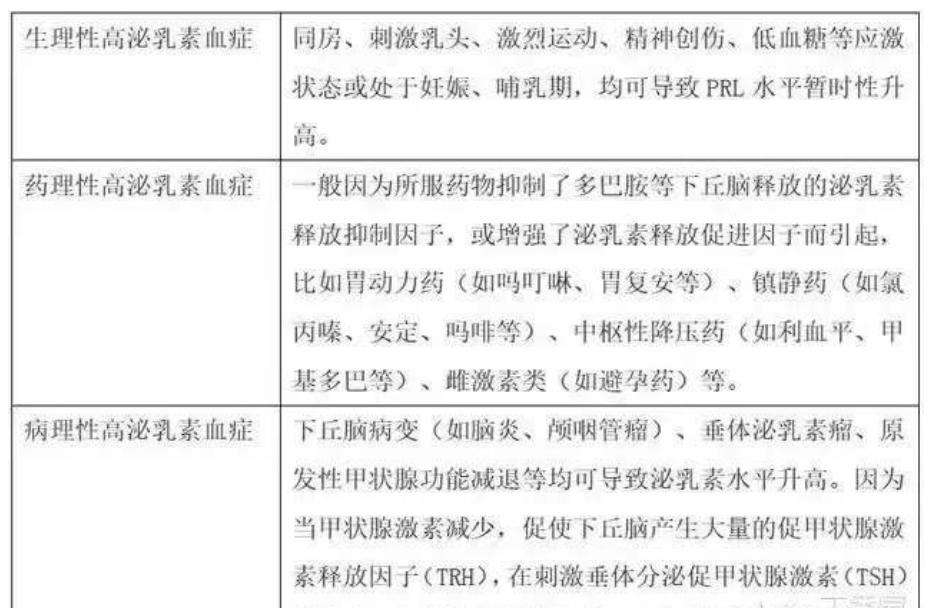
Factors influencing PRL/Image Source: Lilac Garden
- 3 -
Estradiol (E2)
E2, the hormone that dominates women, is the most active estrogen and is secreted by the ovaries and adrenal glands. E2 is mainly secreted by the lower unit of the pituitary gland, the ovaries (non-pregnant), although the birth of the "class" is low, but she has the right to "petition", through positive and negative feedback to regulate the secretion of pituitary hormones (FSH, LH). Combining her with FSH and LH allows for some assessment of ovarian function.
- 4 -
Progesterone(P)
Similarly, the ovaries can also produce progesterone (P), although the ovaries are not the only organs in the body that produce progesterone, but they are large households that produce progesterone during non-pregnancy (the adrenal glands can also produce small amounts of P). P often accompanies E2 to exert a suppressive effect on FSH and LH (negative feedback effect). We use progesterone clinically, mostly to determine whether there is ovulation in this cycle, if no ovulation occurs, P is generally less than 1ng/ml. (In addition, follicular flavinization can also lead to an increase in progesterone, which also needs to be combined with ultrasound, as determined by a specialist doctor.) If basal P is elevated during menstruation, it suggests a possible luteal atrophy.
- 5 -
Testosterone(T)
There is also testosterone (T), derived from the ovaries and adrenal glands, listening to the name, he does not seem to be the home field battle in the female body, but he is a precursor to the body's synthesis of estradiol, under the action of aromatase, gorgeous transformation into estrogen.
These hormones fluctuate greatly in the body at different times. We generally recommend taking blood during menstruation (generally recommended on days 2-5 of the menstrual cycle) to know the underlying endocrine level. It is the "baseline" of observations where we find problems.
3 case studies that teach you how to analyze six reports of sex hormones
Below we will taste a specific case of this "basic" version of this unpredictable hormone.
Case 1: What data will change when ovarian reserve function declines at the age of 39?
The patient, a 39-year-old woman, actively responded to the national policy and prepared to conceive three children. After half a year of no movement, I came to the hospital for treatment.
First of all, we recommend that after the age of 35 and infertility is more than 6 months, relevant tests should be actively carried out. Looking at her basal endocrine, we can observe a lonely increase in basal FSH (bFSH) levels. What does this mean?
In general, abnormally elevated FSH may indicate a decrease in ovarian function. There is currently no cut-off point for FSH as a criterion for predicting hypo-ovarian dysfunction, and bFSH >10IU/L is used as the diagnostic cut-off value in domestic clinical practice [1]. This was confirmed by subsequent ultrasound examinations, which have only 6 double ovarian basis sinus follicles in total (usually less than 5-7 AFCs, suggesting decreased ovarian reserve).
With the increase of age, women's FSH and LH will continue to rise, and FSH and LH will be greater than 40 IU/L to reach the level of menopause. With the repeated postponement of the childbearing age, many patients face the same situation as this woman when they visit the doctor, so it is wise to intervene as soon as possible, and do not envy the fish again.
Case 2: Premature ovarian failure at the age of 24, this data is not ordinary!
The patient, a 24-year-old woman, was diagnosed with a short menstrual cycle due to the fruitlessness of one year of pregnancy.
Let's look at her basal endocrine, FSH, LH have not been elevated, breathe a sigh of relief, is that no problem?
BUT, how did E2 break through the hundred?
At this time, she was given an ultrasound, and on the 3rd day of menstruation, there was a developing follicle with a diameter of 1.1 cm in the right ovary. Prematurely developing follicles, followed by elevated E2, are also manifestations of hypofunction of the ovaries. For this young patient, it is a manifestation of early decline.
Source: Tencent Medical Code She Knows
In general, the reference range of the level of basic E2 in women is relatively wide, generally around 50 pg/mL, and if the E2 level is greater than 80 pg/mL, it reflects the patient's fertility decline. E2 levels greater than 100 pg/mL indicate that ovarian function is not ideal [2].
The same is the decline in ovarian function, why is her FSH not as high as in Case 1?
That's because under the negative feedback of E2, there is no abnormal trend for the time being. When there is no follicle development, E2 secretion is insufficient, and the "flood force" of ovarian function is no longer suppressed, FSH will rise in trend.
Case 3: What is the abnormality of the 32-year-old who got the six items of PCOS sex hormones?
The patient is a 32-year-old woman with irregular menstruation and menstrual cramps for 2-3 months. Ultrasound suggests that both ovarian AFCs are greater than 12. It is diagnosed with "polycystic ovary syndrome (PCOS)".
We look at her hormones, and LH is counter-aggressive compared to FSH levels. Someone said: My LH is not higher than FSH, then it is not PCOS?
In fact, high LH is no longer the standard for diagnosing PCOS, and only about one-third of PCOS patients show typical high LH (LH/FSH≥2), which is more common in non-obese patients.
Increased LH levels increase androgen synthesis, and too much androgen can inhibit follicle development and affect ovulation. Of course, testosterone in patients with PCOS can be manifested as normal or mildly elevated serum total testosterone levels, or low testosterone due to androgen receptor sensitivity, with clinical manifestations of gao xiong, such as hirsutism and acne. Both LH and T can be reduced to ideal levels by taking the pill.
In this patient, there was no significant increase in testosterone, and the LH was slightly higher, because of its 2-month menstrual hypochondria, ultrasound showed the thickness of the intima 6 mm, and progesterone was given to peel off the intima as soon as possible. After menstruation, Yousmin is given regular menstruation.
Xiaobian shares
Girls who are not yet pregnant should not worry, whether the successful pregnancy involves multiple factors such as endometrial environment, embryo quality, and evasion effect, fetal stoppage, repeated implantation failure, repeated abortion, and repeated test tube failure, are all difficult problems in reproductive medicine, and it is necessary to synthesize multidisciplinary opinions for more personalized and fine treatment.
【Reference】
HOU Zhen,LIU Jiayin. Evaluation of female fertility assessment and its influencing factors[J].Journal of Practical Obstetrics and Gynecology,2021,37(10):726-729.
GUO Liping. The Value of Serum Sex Hormone Detection in the Clinical Diagnosis of Infertility and the Impact of LH Level[J]. Journal of Shanxi Health Vocational College,2020,05:72-73.]
Source: Reproductive Medicine Space
Editor: Ren Mileage Reviewer: Xiao Ran