Wen 丨 Chen Gen
Helicobacter pylori is definitely one of the most talked about health topics in recent days, as evidenced by the frequency with which it has been searched for. Concern about Helicobacter pylori seems to be on the rise as never before.
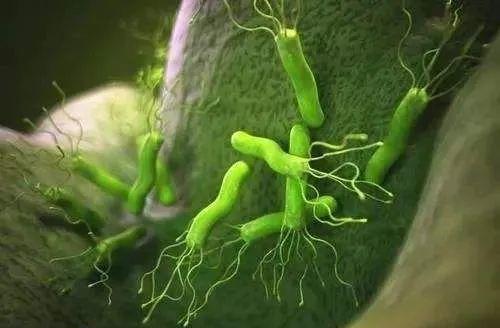
As a gram-stained negative spiral-shaped bacterium, Helicobacter pylori is transmitted from person to person primarily through the mouth-to-mouth route. Once it enters the human body from the mouth and colonizes it, it is difficult for the human body to remove spontaneously, resulting in long-lasting or lifelong infection. Helicobacter pylori infection can almost always cause active inflammation of the gastric mucosa, and on the basis of chronic inflammatory activity, some patients can also develop a series of diseases such as peptic ulcer and gastric cancer.
Although Helicobacter pylori has become one of the important research areas in the scientific community since its discovery, in the long run, even if scholars and experts try to popularize the possible harm that Helicobacter pylori can cause to the human body, Helicobacter pylori infection has rarely attracted people's attention. For Helicobacter pylori infection, at least for now, getting attention and getting into discussion is always a good start.
Helicobacter pylori and stomach cancer
The discovery of Helicobacter pylori is of great significance.
In 1983, Australian scholars Marshall and Warren successfully isolated and cultured a curved and S-shaped bacterium on the gastric mucosa of patients with gastritis and peptic ulcer, and named it Campylobacter pylori. In 1989, the study found that the bacterial gene sequence and biochemical characteristics were different from the previous Campylobacter genus, so it was divided into a new genus, named Helicobacter pylori.
For this achievement, the two scholars won the 2005 Nobel Prize in Physiology and Medicine, which also proved the clinical significance of the discovery of Helicobacter pylori.
It should be known that in the past view, the high acid environment in the stomach is not suitable for bacterial growth, but the cultivation of Helicobacter pylori has successfully subverted the traditional concept and become an important milestone in the history of human medicine - Helicobacter pylori is the only microbial species known to survive in the strong acid environment of the human stomach. It can parasitize the human stomach, adhere to the gastric mucosa and cell spaces, and neutralize stomach acid by constructing an alkaline microenvironment.
In addition to being associated with chronic gastritis and peptic ulcer, the spectrum of infection-related diseases of Helicobacter pylori infection has expanded greatly after the discovery of Pylori. Helicobacter pylori infection can cause lymphoma of gastric mucosa-associated lymphoid tissue, which is the cause of dyspepsia in some patients and a prerequisite for the development of enteropathic gastric cancer. In addition, its infection is also associated with some parenteral diseases. Among the diseases associated with Helicobacter pylori infection, chronic gastritis, peptic ulcer and stomach cancer are common diseases. It can be said that Helicobacter pylori infection constitutes a large burden of disease.
Not long ago, the U.S. Department of Health and Human Services released the 15th edition of the Carcinogen Report, adding 8 new carcinogens. Among them, chronic infection of Helicobacter pylori was listed as a class of carcinogens for the first time. You know, stomach cancer is one of the most common digestive tract tumors in China, and about half of the world's stomach cancer cases occur in China.
According to the data of the National Cancer Center, in 2015, the incidence of gastric cancer in China ranked second among all malignant tumors, with 679,100 new cases and 498,000 deaths, and Helicobacter pylori infection is the main cause of stomach cancer in China. More than half of Chinese are infected with Helicobacter pylori, and even among people under 20 years of age, the infection rate is as high as 37.1%.
Last month, Lancet published a study of stomach cancer in Chinese populations. The results showed that the higher the education, the higher the incidence of Helicobacter pylori infection, and the overall infection led to a nearly 6-fold increase in the risk of non-cardia gastric cancer in Chinese, and an increase of about 3-fold in the risk of cardia cancer.
Specifically, the study used samples from the China Kadoorie Biobank, and after 10 years of follow-up, the incidence of non-cardia gastric cancer (where the cardia is located in contact with the esophagus and the stomach) was 57.6 per 100,000 person-years, and the incidence of cardia cancer was 10.5 per 100,000 person-years, both of which increased with age, with the incidence in men about 3 times that of women. The rate of Helicobacter pylori infection in patients with non-cardia gastric cancer was 94.4%, 92.2% for cardia cancer, and 75.6% for the general population.
Subsequently, the researchers changed the detection of Helicobacter pylori infection from western blot analysis to the current clinical method. The positive rate of Helicobacter pylori in patients with non-cardia gastric cancer after the change was 84%, 80% for cardia cancer, and 58% for the general population. The risk ratios were 4.68 times (non-cardia gastric cancer) and 2.36 times (cardia cancer), respectively. Consistent with the conclusions before changing the method.
That said, whether it is non-cardia stomach cancer or cardia cancer, Helicobacter pylori infection is a huge risk factor for Chinese group of stomach cancers. It shows that about 80% of non-cardia stomach cancers and more than 60% of cardia cancers are caused by Helicobacter pylori infection.
From the dining system to the divided meal system
While the harm of Helicobacter pylori infection is becoming more and more popular to the public, what people still need to do is to take corresponding measures to prevent Helicobacter pylori infection.
There is a general susceptibility to Helicobacter pylori in the population, but the majority of Helicobacter pylori infections occur in childhood. The infection rate of Helicobacter pylori in children in China is 25% to 64%, which increases at a rate of 0.5% to 1% per year, and the growth rate gradually slows down from rapid to 50 to 60 years old. The infection rate of Helicobacter pylori in elderly patients with gastrointestinal diseases even exceeds 70%.
From the perspective of the source of infection, humans are currently the only clear source of helicobacter pylori infection, and "mouth-to-mouth" transmission is the main transmission route of Helicobacter pylori at present. According to the current statistics, about half of the people in the world have been infected with Helicobacter pylori, and the infection rate of Helicobacter pylori in different countries and regions and different ethnic groups is very different, mainly related to living habits, living environment, eating habits, public health conditions and water supply.
The rate of Helicobacter pylori infection increases with age, as well as a decrease in immunity. In developing countries, the infection rate of Helicobacter pylori is relatively high, about 50%-80%; in developed countries, the infection rate of Helicobacter pylori is low, about 25% to 50%; the average infection rate in China is about 50%, it can be said that one in every two people is a carrier of Helicobacter pylori. The reason why there is such a large number of Helicobacter pylori infection population in China is mainly due to our traditional eating habits of not using public chopsticks.
Just as the so-called disease comes from the mouth, the meal is the eating habit left by our Chinese culture for thousands of years, that is, everyone eats together, tableware, food are shared, and the chopsticks that come out of the mouth of a table of people are not happy in the same dish, which creates natural conditions for the infection of Helicobacter pylori. This is why Helicobacter pylori infections are usually family and familial, especially in close relationships.
In fact, close contact, especially between parents and children within the home, may be a very important factor in Helicobacter pylori infection. Studies have reported that compared with families without Helicobacter pylori infection, the relative risk of child infection with Helicobacter pylori infection in the case of a mother is positive for Helicobacter pylori infection is 8 times that of the control group, and in the case of a positive Helicobacter pylori infection in the father, the relative risk of infection of Helicobacter pylori in the child is 4 times that of the control group.
Needless to say, in order to reduce the incidence of stomach cancer, it is necessary to fundamentally control the infection of Helicobacter pylori. Theoretically, as long as this bacterium is not allowed to enter the mouth, it can be prevented, but obviously, it is not enough to prevent Helicobacter pylori by itself, and the family treats at the same time, disinfects the dishes and chopsticks, uses public chopsticks and meals, pays attention to oral hygiene, and regularly changes the toothbrush is the most critical measure to prevent the infection of the bacteria.
Among them, in addition to the use of tableware for parents and children, parents and children should not only use separately, but also abandon the habit of feeding infants and young children in a mouth-to-mouth manner or giving chewed food to children. In addition, if the tableware is recycled during meals, it may also infect Helicobacter pylori if it is not disinfected in time. Therefore, when eating out, you should also pay attention to safety and hygiene, and maintain good eating habits.
Of course, from a preventive point of view, the Helicobacter pylori vaccine should be the most ideal preventive measure. In fact, since the 1990s, scientists have been working on developing a vaccine against Helicobacter pylori. In animal experiments, the Helicobacter pylori vaccine can achieve preventive and therapeutic results in preventing Helicobacter pylori infection.
Professor Zou Quanming's research group of the Third Military Medical University used the urease B subunit fusion of the heat-sensitive enterotoxin B subunit to develop an oral recombinant Helicobacter pylori vaccine, which was verified in a phase 3 clinical trial. After vaccination, the effective rate was 71.8% within 1 year, 55.0% in 2 years, and 55.8% in 3 years. Of course, Helicobacter pylori infections mostly occur in childhood. Therefore, ideally, the vaccine needs to be protected for 10 to 15 years or more, and the vaccine at this stage still needs to face a series of technical problems.
High disease burden
Let's look at the treatment again. After all, among the residents of Our country, the infection rate of Helicobacter pylori is as high as more than 50%. In addition, due to the socio-economic level, public health conditions and water supply and other factors, the rural infection rate has reached more than 60%. The huge population base and the aging trend of society make Helicobacter pylori infection and related diseases a remarkable public health problem in China, constituting a high burden of disease.
Obviously, according to the above ratio, there should be a considerable part of the population that needs to be treated for Helicobacter pylori infection. The expert consensus released by China in 2021 also pointed out that it is recommended to give eradication treatment to all adult Helicobacter pylori infection in the family. Because intra-family transmission is the main route of infection in children with Helicobacter pylori, and most Helicobacter pylori infections occur in childhood and adolescence, the level of infection in 12-year-old children is close to that of adults.
But the reality is that although people are gradually understanding the harm that Helicobacter pylori may cause to the human body, there is still no strong awareness of prevention and treatment. Therefore, large-scale screening and eradication of Helicobacter pylori should be considered as a key strategy for preventing stomach cancer in China, as it is clear that there will be huge health benefits.
At the same time, as an infectious disease, helicobacter pylori infection should be the best treatment method based on susceptibility testing, but the feasibility, cost-benefit ratio, reliability and in vivo and in vitro consistency of susceptibility testing limit the wide application of this treatment method. Therefore, empiric treatment based on local antibiotic resistance rates, antibiotic consumption and clinical trial results is the mainstay of treatment for clinicians today. Of course, whether individualized or empiric, drug availability, treatment costs, and potential adverse effects should be taken into account.
In addition, helicobacter pylori infection is not easily eradicated because most antibiotics have reduced activity in a low pH environment in the stomach and cannot penetrate the mucus layer to reach bacteria. To date, no single drug has been effective in eradicating Helicobacter pylori. Therefore, medical treatment regimens have also been developed in combination with antacpressants, antibiotics or bismuth agents that play a synergistic role.
In today's rapid development of modern medicine, we are increasingly concerned about the quality of life, and the long-term benefits of treating Helicobacter pylori to reduce the risk of stomach cancer are becoming clearer. This requires us to get rid of the influence of various false rumors and strive to carry out a standardized treatment. Attention is already a good start, and we look forward to more good progress.