▎ WuXi AppTec content team editor
Thyroid cancer is a malignant tumor with the highest incidence in the endocrine system, which is mainly divided into papillary carcinoma, follicular carcinoma, undifferentiated carcinoma and medullary carcinoma. The incidence of thyroid cancer has been increasing worldwide in recent decades.
Is there indeed an increase in morbidity, or is overdiagnosis increasingly common? Recently, The Lancet Diabetes & Endocrinology published a blockbuster analysis study. Based on the GLOBOCAN database, the study provided an in-depth analysis of age-standardized incidence and mortality of thyroid cancer in 185 countries or regions in 2020, and dissected the complexities and potential risk factors behind the increasing number of thyroid cancers, as well as more appropriate treatment methods.
The results show that although there are significant differences in the incidence of thyroid cancer in different countries and regions around the world (such as the incidence of thyroid cancer in women can be 15 times different), at the same time, the mortality rate of thyroid cancer patients remains low, and the mortality data of different countries and regions are similar.
The concurrent comments of the paper pointed out that the epidemiological characteristics of global thyroid cancer shown in the current study strongly reflect the existence of overdiagnosis of thyroid cancer, and overdiagnosis of thyroid cancer has become an important global public health problem!
Screenshot source: The Lancet Diabetes & Endocrinology
The global status of thyroid cancer: high incidence and low mortality
The paper points out that in the past few decades, the epidemiological status of thyroid cancer in some countries and regions has shown the characteristics of high incidence and low mortality, which strongly suggests that thyroid cancer may be overdiagnosed clinically.
Based on the GLOBOCAN database, the current research team further analyzed the epidemiological characteristics of thyroid cancer in 185 different countries and regions around the world in 2020, with different sexes and different age groups (0-4, 5-9 、...、 80-84, ≥ 85 years old, a total of 18 age groups).
The results of the study show that:
Overall, there were 449,000 and 137,000 newly diagnosed thyroid cancer patients in women and men in 2020, respectively, and the age-standardized incidence rates for women and men in the global population were 10.1/100,000 and 3.1/100,000, respectively;
Approximately 44,000 people worldwide (28,000 women; 16,000 men) died of thyroid cancer globally in 2020, with age-standardized thyroid cancer mortality rates of 0.5/100,000 and 0.3/100,000, respectively, among women and men;
Countries with a high level of economic and social development have a significantly higher incidence of thyroid cancer. However, the mortality data for thyroid cancer in different countries and regions are low and similar;
The incidence of thyroid cancer in women in different countries and regions around the world can vary by up to 15 times, and the incidence of thyroid cancer in men in different countries and regions around the world also varies greatly, but compared with women, the difference is relatively small.
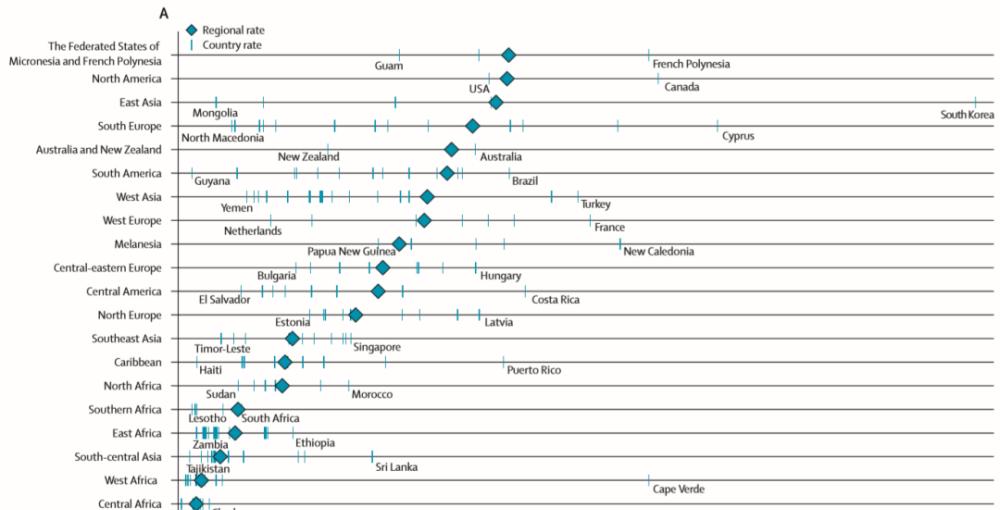
▲The age-standardized incidence of thyroid cancer in women in different countries and regions can vary by up to 15 times (Image source: Reference[1])
The paper notes that the research data strongly reflect the presence of overdiagnosis of thyroid cancer. Overdiagnosis means that some thyroid cancer patients do not develop severe symptoms or die without treatment if they are not detected by testing.
What factors are associated with overdiagnosis?
The paper pointed out that the over-diagnosis of thyroid cancer is related to the widespread application of cervical radiographic detection technology (such as neck ultrasound, ultrasound detection of arteries above the aortic arch and CT, etc.) in recent years, and neck imaging technology supplemented by fine needle puncture cytology has made more and more thyroid cancer detected, and the incidence data of thyroid cancer began to grow.
The results of autopsy studies suggest that some patients who die from non-thyroid cancer have tiny thyroid papillary carcinoma, which is a common differentiated thyroid cancer, slow growth and mild malignancy, generally no more than 2 cm in diameter, this part of the population will not know that they have thyroid cancer if they do not perform autopsy for a lifetime.
The difference in thyroid cancer incidence between men and women is mainly due to the diagnosis of tiny thyroid papillary carcinoma (<2 cm), and the ratio of the incidence of minimal thyroid papillary cancer in women to male incidence is 4.4:1.
Overdiagnosis allows a large number of "latent" asymptomatic thyroid cancer patients to be detected. In addition to tiny papillary thyroid cancers, patients with larger thyroid cancers may remain asymptomatic for a long time, and these patients are occasionally diagnosed by imaging tests for other diseases.
How can over-diagnosis and treatment be avoided?
The only clear risk factor for thyroid cancer is exposure to ionizing radiation, especially in childhood. Scientists have also proposed many other possible risk factors, such as exposure to endocrine-damaging chemicals, obesity, and genetic predisposition factors. However, the influence and extent of these factors need to be further confirmed by more studies on the basis of controlling for potential bias factors.
The concurrent review of the paper pointed out that the overdiagnosis of thyroid cancer has become a global public health problem that should be limited. For the population as a whole, overdiagnosis of thyroid cancer can lead to unhelpful overtreatment.
Avoid overdiagnosis:
For asymptomatic people who do not have associated risk factors for the disease, current guidelines do not encourage cervical ultrasound in such populations. When an individual's thyroid nodule is more than 1 cm in diameter, a fine needle aspiration cytology of the suspected nodule may be considered.
Avoid overtreatment:
In addition, we should also limit overtreatment of thyroid cancer. For people with papillary thyroid cancer with lesions less than 1 cm in diameter, active monitoring and surgical treatment only when the tumor progresses (tumor volume increases or suspicious lymph nodes appear) can achieve similar results to immediate surgery.
For low-risk thyroid cancer populations, limited treatment with adenectomy is recommended when the lesion is only unilateral, and exemption from postoperative radioactive iodine therapy may be considered when treating with thyroidectomy.