Recently, ICU consulted several cases of pan-resistant or fully resistant Acinetobacter Baumannii, there are fixed value bacteria and pathogenic bacteria, some use tigecycline to control infection, there are also use of tigecycline combined with polymyxin B and other antibacterial drugs are still uncontrollable serious infection, the patient's high fever does not go away, serious infection caused multi-organ failure, and eventually died because the infection can not be controlled. As a healer, I feel deeply confused and panicked.
So what kind of superbug is Acinetobacter baumann? How can we treat this superbug? How should we prevent nosocomial infections?
Acinetobacter baumannii: superbugs bred by antibiotics
Acinetobacter baumannii is the most common gram-negative bacillus in the genus Acinetobacterium, which is widely present in water and soil in nature, as well as in normal human skin, respiratory tract, digestive tract and genitourinary tract, and is a conditional pathogenic bacteria. The bacteria are widely distributed in the hospital environment and can survive for a long time, which is very easy to cause infection in critically ill patients, so it is often isolated from the blood, urine, pus and respiratory secretions of infected patients.
Acinetobacter baumann can cause hospital-acquired pneumonia, bloodstream infections, intra-abdominal infections, central nervous system infections, urinary tract infections, skin and soft tissue infections, etc. According to chinet's continuous drug resistance surveillance, Acinetobacter is located in the third place for clinical isolation of gram-negative bacteria in large teaching hospitals in mainland China [1]. According to the results of the 2017 National Drug Resistance Monitoring Report, the resistance rate of Acinetobacter baumannii to carbapenems is close to 70%, respectively, which is higher than in 2016 [2].
In hospitals, contaminated medical devices and the hands of Acinetobacter baumann staff are important vectors of communication. Susceptible patients are elderly patients, premature babies and newborns, surgical trauma, severe burns, tracheostomy or intubation, use of artificial ventilators, intravenous catheterization and peritoneal dialysis, broad-spectrum antibacterial drugs or immunosuppressants, etc.
2. How to treat Acinetobacter baumannii?
First, clarify the classification of drug resistance:
Multidrug-resistant Acinetobacter (MDRAB) refers to three or more classes of antibacterial drugs that have antibacterial activity against the bacterium;
Acinetobacter xenophotoseum (XDRAB) refers to strains that are sensitive only to tigecycline and / or polymyxin;
Totally resistant Acinetobacter (PDRAB) refers to strains that are resistant to all antimicrobials currently available on the mainland [1].
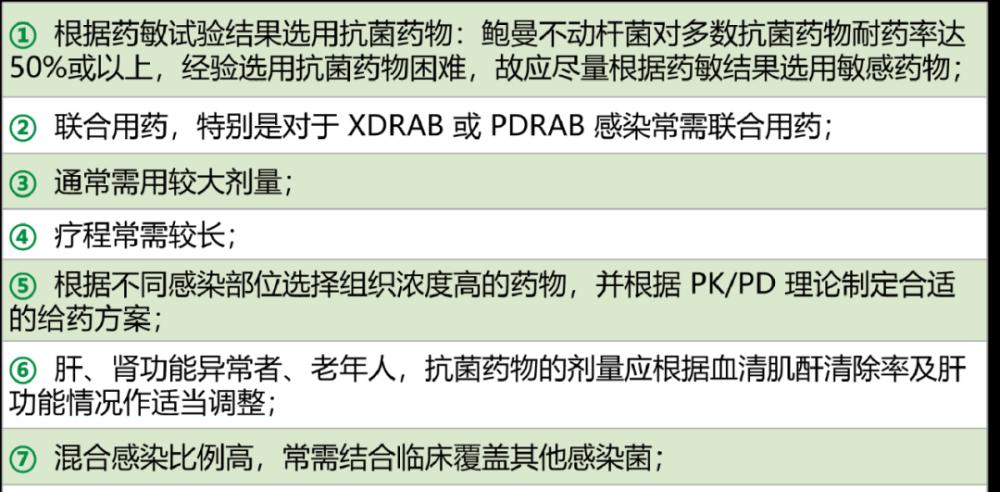
(1) Principles of antibacterial treatment of Acinetobacter baumannii infection (AB).
The sensitivity of the pathogen, the location of infection, the severity, the pathophysiology of the patient, and the characteristics of the action of antibacterial drugs should be considered comprehensively. The main principles are as follows [1]:
(2) Acinetobacter baumann infection (AB) commonly used antibacterial drugs
(3) Acinetobacter baumannii MDRAB, XDRAB or PDRAB infection commonly used combination drugs
MDRAB infection: sulbactam β lactamase inhibitor complex or carbapenem antibiotics can be selected according to the results of susceptibility, and aminoglycoside antibiotics or fluoroquinolone antibacterial drugs can be used in combination.
Common combination regimens for XDRAB infection:
In anti-infective therapy, even if the drug susceptibility alone suggests carbapenem resistance, drug resistance does not equal complete ineffectiveness, but still needs to be combined administration, carbapenems such as meropenem, increasing the frequency of administration, increasing the dose of administration, prolonging the instillation time can overcome low levels of drug resistance.
(4) Treatment course of Acinetobacter baumannii infection
The course of treatment depends on the severity of the infection, complications, and resistance of the pathogen.
How to prevent nosocomial infections?
Most of the nosocomial infections of Acinetobacter baumannii are exogenous nosocomial infections, and their transmission route is mainly contact transmission, so it should be managed as follows:
(1) Strengthen the management of hand hygiene hospitality: Good hand hygiene can significantly reduce the incidence of drug-resistant bacteria infection and colonization incidence, which is one of the key measures to reduce the occurrence of hospital infection [4].
(2) Standardize the collection and examination, and correctly interpret the microbial test report: For cases clinically diagnosed as bacterial fungal infection, a qualified microbial specimen of the infected site should be collected in time before starting antibacterial therapy and sent for pathogenic testing [5].
(3) Reduce the irrational use of antibacterial drugs: supervise and manage the clinical application of tigecycline and carbapene special antibacterial drugs, strictly implement the requirements for antibacterial drug classification and physician prescription rights management; encourage clinical pharmacy departments to actively carry out drug concentration monitoring and pharmacokinetic (PK)-pharmacodynamic (PD) related research, and eliminate the use of drugs that do not conform to the PK/PD principle. Doing a good job in the clinical application management of antibacterial drugs is an effective measure to promote the rational use of antibacterial drugs and curb bacterial resistance and the infection caused by it.
(4) Contact prevention [2]: Medical staff, family members and accompanying personnel who come into contact with drug-resistant bacteria infection / colonization of patients should correctly implement contact precautions: including wearing personal protective equipment, equipment-specific, restricting patient transport and standardizing the management of medical waste.
(5) Strengthen environmental cleaning and disinfection.
bibliography:
[1] Zhou Hua, Zhou Jianying, Yu Yunsong. Interpretation of the Consensus of Experts on the Diagnosis, Treatment and Prevention of Acinetobacter Baumann infection in China, Chinese Journal of Evidence-Based Medicine, 2016, 16(1): 26~29.
[2] Technical Guidelines for The Prevention and Control of Gram-Negative Bacillus (CRO) Infection in China, Chinese Journal of Hospital Infectious Diseases, 2019, 29(13): 1921-1926
Xu Yingchun, Xiao Yonghong, Zhuo Chao, et al. Epidemiology and prevention and control strategies of carbapenem-resistant Enterobacteriaceae bacteria in China[J]. Chinese Practicing Pharmacist.2013,10(4):3-8.
Huang Xun, Deng Zde, Ni Yuxing, et al. Chinese expert consensus on hospital infection prevention and control of multidrug-resistant bacteria[J]. Chinese Journal of Infection Control,2015,14(1):1-9.
National Health and Family Planning Commission of the People's Republic of China. Guidelines for the Clinical Application of Antimicrobials (2015 Edition).
Typography: Super League
This article was first published on Lilac Garden's professional platform: Breathing Time