Bladder cancer is a malignant tumor caused by the malignant proliferation of bladder cells, and the risk of disease in men is more than 3 times that of women, and its risk of developing the disease increases with age. Depending on the degree of invasion, it can be divided into invasive bladder cancer and non-invasive bladder cancer. The current treatment measures are mainly surgery, combined with chemotherapy, immunotherapy and other methods.
Treatment of invasive bladder cancer is generally platinum-based chemotherapy. Due to the rise of immunotherapy, immunotherapy represented by PD-1 inhibitors has made great efforts in the field of bladder cancer treatment. KEYNOTE-045 studies have shown that patients with bladder cancer can achieve a better benefit if their condition progresses after chemotherapy in the first line, and the use of immune checkpoint inhibitors on the second line. If the patient's tumor tissue sample pD-L1 expression is relatively high, it is possible that the treatment with immune checkpoint inhibitors will be more effective, although this conclusion is still controversial.
Let's first look at a case report related to it.
PD-1 inhibitors treat bladder cancer with long-term remission
A 69-year-old Japanese man seeks medical treatment for hematuria. The patient had non-muscle invasive bladder cancer at the age of 57 and was treated with transurethral bladder tumor resection, with the pathological result of carcinoma in situ in the bladder diverticulum, after which no other treatment was received after surgical resection.
After a lapse of 12 years, the patient developed hematuria again, and an MRI diagnosis was found to be local invasive T4 bladder cancer, and the tumor invaded the branch of the internal iliac artery that developed from the diverticulum. After surgery, high-grade invasive urothelial carcinoma was found, and patients refused total cystectomy and opted for treatment with a preserved bladder.
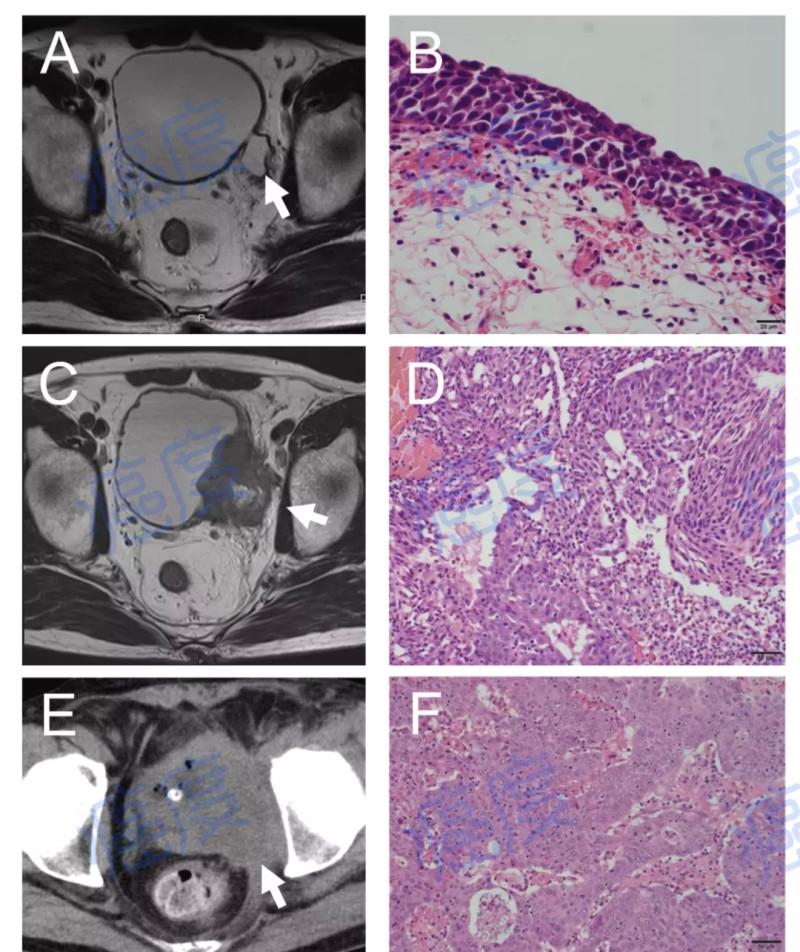
Figure 1: Imaging and pathological examination results after radiation therapy
Chemotherapy with cisplatin plus gemcitabine was first performed, plus radiation therapy. However, tumor residues were still found after treatment, so the patient received a combination of methotrexate, vinblastine, epirubicin, and carboplatin, which is the second-line treatment regimen. However, this regimen did not work, the disease still progressed rapidly, and patients presented with pain and swelling in the left leg.
It so happened that Japan approved the marketing of the PD-1 inhibitor pambolizumab at this time, so patients began to use pambolizumab for treatment. After six courses of treatment, CT imaging revealed a 50% reduction in tumors, which was clinically assessed as partial remission. After nine courses of treatment with PD-1 inhibitors, repeated bladder irrigation is required due to recurrent occurrences of necrotic tissue leading to urinary retention.
Due to the problem of urinary retention, the patient underwent treatment for ureteral cutaneous fistula without resection of the whole bladder. After the operation, the necrotic tissue disappeared. After six more courses of PD-1 inhibitor therapy, the tumor completely subsided. Clinical evaluation for complete remission.
After 20 courses of PD-1 inhibitors, patients developed adverse reactions of ACTH (adrenocorticotropic hormone) deficiency, rash and other immunotherapy, so the patient stopped using pambolizumab. Although PD-1 inhibitors were discontinued, patients have been in complete remission for more than 24 months, indicating a longer-term survival benefit.
Figure 2. Imaging and pathological outcomes after PD-1 treatment
Later researchers tested the PD-L1 expression of the patient's biopsy at different stages and found that the initial PD-L1 expression of the patient was negative; in the chemoradiation stage, the patient's tumor tissue sample pD-L1 expression was positive, which was 5%, and after the end of chemoradiation, the PD-L1 expression exceeded 10%.
revelation
Summarizing this treatment case, we found that the time of use of PD-1 inhibitors in this patient was relatively coincidental, and at the time of initial treatment, PD-1 inhibitors were not yet available in Japan, and the patients used two stages of chemotherapy successively, and the treatment effect was not ideal. After testing, the expression of PD-L1 in the initial tumor tissue of the patient was negative, and PD-L1 began to be expressed after the killing of tumor cells by means of pre-radiotherapy and chemotherapy. At this time, when PD-1 inhibitors were listed in Japan, patients began to take effect with PD-1 inhibitors and obtained better treatment results.
When many patients choose a treatment method, they always mistakenly think that the most advanced must be the best, which can quickly alleviate or even cure their own pain. The traditional radiotherapy and chemotherapy, in the patient's mind, not only has great toxic side effects, but also does not necessarily have an effect, so it will subconsciously reject these treatment methods.
However, there are great individualized differences in the treatment of tumors, which treatment methods to choose, which drugs can be combined, and professional doctors need to make decisions according to the actual situation of patients in order to achieve the best treatment effect. At present, the treatment of many solid tumors is actually limited, and we must find ways to maximize the effect of each means and drugs and achieve the greatest benefit as much as possible.
参考文献:Yuki Horibe, et al., A case of long-term complete remission of locally advanced T4 bladder cancer treated with pembrolizumab. Urology Case Reports 41 (2022) 101959.