Ground glass nodules are common, some of which are lung cancer, and surgery is needed as soon as possible to cure them.
First show you a simple, rely on CT film can be diagnosed, the difficulty is not easy to learn will be:
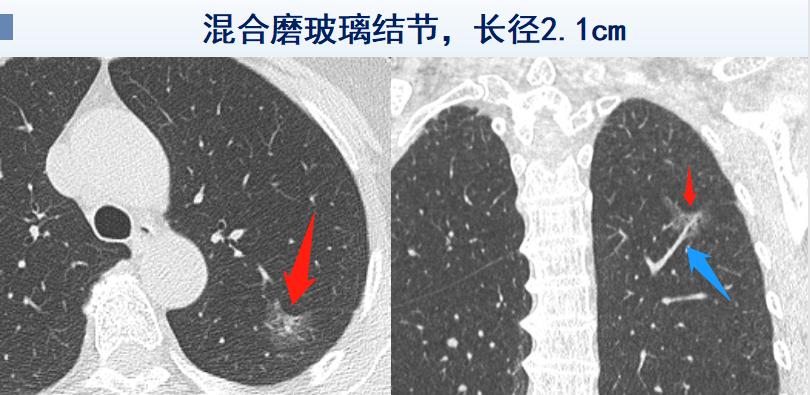
2.1cm mixed ground glass nodules
This is a middle-aged lady, after a cold intermittent cough, a bout of light and heavy, took cough medicine does not work, did a CT examination, the result of the doctor said that she had a small thing in her lungs, to perform a small operation to take it out and throw it away.
After opening the patient, the doctor explained to her husband: This is an early lung cancer, lung adenocarcinoma, recommended surgery, the treatment effect will be very good.
What is the basis for the doctor's diagnosis?
A: Mixed ground glass nodules are more than 1.5 cm, accompanied by pleural depression (red arrows), vascular passage, and the blood vessels are stiff and blurred.
Why should surgery be recommended as soon as possible? Because the solid component of this ground glass nodule is in contact with the interlobeal pleura and also to the penetrating blood vessels. When the solid composition inside the mixed polished glass nodule is greater than 5mm and the boundary is not clear, it is necessary to be vigilant against cancer cell infiltration, at which time there is a way to spread, and it is not appropriate to stay for a long time.
Later, the woman went to the thoracic surgery department for minimally invasive surgery, and the case was a micro-invasive adenocarcinoma.
This condition does not require follow-up adjuvant therapy, and regular review is enough.
Lung nodules are actually very common, and cross-sectional studies of screening populations have shown that the detection rate of lung nodules ranges from 2.1% to 64.5% (different regions, age, occupation, smoking history factors, etc., vary greatly), but the detection of ground glass nodules is not equivalent to the detection of early lung cancer, and the detection rate of early lung cancer in screening populations is 0.45% to 2.1%.
In the Asian population, patients are mostly non-smoking women, most are asymptomatic, and up to 20% of patients have multiple nodules.
That is to say, lung nodules are very common, benign far more than malignant, but timely identification of malignant lung nodules can terminate the development of lung cancer, which is the significance of our attention to the chest health examination of high-risk groups.
Some doctors have concluded that 90% of long-standing ground glass nodules are neoplastic lesions.
Therefore, people who have examined a ground glass nodule in the lungs need to identify two problems:
1. Is the nodule benign or malignant?
2. Should the nodule be surgically removed?
Below we use several case classifications to explain, but also to teach you to learn the CT diagnosis of ground glass nodules, it is not difficult!
1. How to identify malignant ground glass nodules?
Ground glass nodules, refer to diameter
The above three are ground glass nodules, the left picture is pure grinding, the middle and right pictures are mixed ground glass nodules, these three patients are regularly reviewed nodules without absorption, and later undergone minimally invasive surgical resection, the cases are carcinoma in situ, micro-invasive adenocarcinoma and invasive lung adenocarcinoma.
Common malignant signs of ground glass nodules are: vacuole sign, lobe sign, pleural depression sign, bronchial inflator sign, bronchial truncation sign, vascular translusion sign (with vascular thickening, stiffness, blurred and other changes).
For example, this 1.5 cm nodule, the edge is divided like a leaf, there are several small black vesicles (vacuole sign) inside, he reviewed the nodule several months apart and did not absorb it, decisively underwent surgery, the pathology is in situ adenocarcinoma (1.5 cm in situ carcinoma is rare, > 1.5 cm is mostly invasive adenocarcinoma).
To briefly explain the vacuole sign, in the early stage of lung cancer, due to cancer cell infiltration, the alveolar spacer elasticity decreases and collapses, and the adjacent alveolar lumen fuses to form a small air cavity visible to the naked eye (but there are also about 5% of inflammatory nodules that can appear vacuole signs, which require comprehensive analysis.
The patient is a mixed ground glass nodule, with many malignant signs, including lobe signs, vascular translucency signs, pleural traction, and the internal white solid composition is not clearly distinguished from the ground glass.
In addition, everyone looks at its blood vessels through, when the white dendritic blood vessels enter the inside of the nodule, it becomes thicker, stiffer, and some of the edges are blurred.
He later underwent minimally invasive surgery, the pathology of which was invasive lung adenocarcinoma.
2. Which lung nodules are the most dangerous and should be operated on as soon as possible?
A lot of people care about this question, but in reality the answer isn't the only one.
Malignant lung nodules (lung cancer) do not develop at a consistent rate, and the speed varies greatly.
In general, aggressive management is recommended for nodules with clear signs of malignancy, or for ground glass nodules that follow up with progression.
Like this 1.4 cm mixed ground glass nodule, which progresses rapidly within 10 months, the surgical pathology is invasive lung adenocarcinoma.
In fact, the timing of his surgery can be further advanced.
Some people like to be a little more rigorous, and you can refer to the following guidelines:
Picture from the network, thanks, invasion and deletion
Note: GGN: ground glass nodules; pGGN: pure ground glass nodules; PSN: partial solid nodules; SN: solid nodules.
A prospective study in South Korea showed no significant differences in recurrence-free survival and overall survival time in patients with imaging non-invasive ground glass nodules (solid component ≤5 mm), immediate surgery and delayed surgery (follow-up only found ground glass nodule growth), and the effect of delayed surgery on long-term survival was small.
I am Dr. Hao of Imaging, I hope that the cases in this article can deepen your understanding of lung nodules, welcome your attention!