Lung hypoplasia and lung hypoplasia
01
Case 1
Brief medical history, female, 64 years old, chest tightness for 2 months, cough, sputum production with fever for 3 days.
As seen in the image:
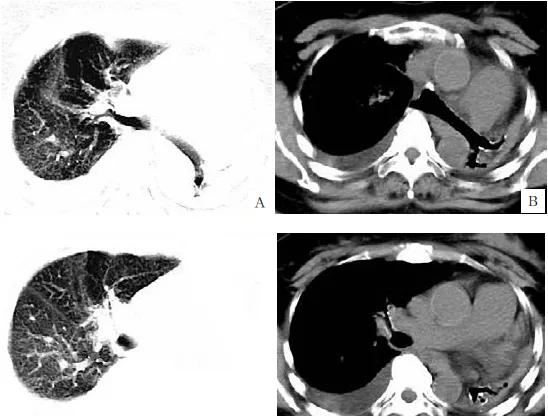
Figures A and C: Chest CT scanned the lung window, showing a flaky density increased shadow of the left lung, of which only a small amount of bronchogram was seen,
The texture of the right lung increased and thickened, and the shadow scattered in the cord and the patchy blurred density increased, the brightness of the right lung part increased, and the cystic translucent lung-free textured area was seen. Figs. B and D: The mediastinal window shows bilateral thoracic symmetry, normal bilateral intercostal space, left lung atrophy, only a small amount of bronchogram seen inside, cylindrical blind end on the distal side, mediastinum and trachea shifting to the left. A small effusion is seen in the right pleural cavity.
Diagnosis: left lung hypoplasia, with mediastinal hernia formation, partial compensatory emphysema in the right lung, and a little inflammation of the right lung, right pleural effusion.
Postoperative pathology (Figure E) was confirmed as left lung hypoplasia and atelectasis.
02
Case 2
Brief medical history, male, 50 years old, cough, sputum cough for 1 week.
Figures A, C, E: CT sweep axial position and coronal position show that the right lung tip sees a small number of clear realm patches and cord shadows, the right lung mid-lobe bronchi is not shown, the right lung middle lobe and lower lobe are withered and see multiple cystic and beaded gas density shadows, different sizes, flaky solid shadows around the surrounding area, and the brightness of adjacent lung tissue is increased. Figures B, D, F: CT pan-scan axis and coronal position show the absence of the right middle lung bronchus, the right middle and lower lung volume reduction, showing a triangular soft tissue density shadow, seeing multiple cysts and columnar dilation bronchi, distal with a dilated cylindrical blind end, and the mediastinum slightly displaced to the right.
Preliminary diagnosis of imaging: right middle and lower lung hypoplasia, secondary bronchiectasis, partial compensatory emphysema of the right lower lung.
Pathological diagnosis: postoperative pathology confirmed as: right middle and lower lung hypoplasia
overview
Lung insplasia and hypoplasia of the lung are caused by lung bud development disorders at a certain stage in the embryonic development process, which is a rare congenital malformation, most of which are complicated by other developmental defects, and the more common ones are pulmonary artery hypoplasia and lack, cardiovascular development deformities, congenital diaphragm hernia and spinal dysplasia.
Lung insanity or lung hypoplasia can be divided into the following pathological types: (1) lung nondevelopment; (2) Pulmonary hypoplasia; (3) Lobe hypoplasia. Recurrent respiratory tract infections of unknown cause should be considered for the presence of congenital pulmonary hypoplasia, diagnosis requires great caution, x-ray is preferred, and MSCT and pulmonary artery perfusion scans can generally be used to determine the cause in those who cannot be confirmed.
Imaging manifestations of pulmonary hypoplasia and pulmonary hypoplasia are as follows.
X-ray: (1) One side of the lung is not developed: on the X-ray chest x-ray chest x-ray, the density of the chest cavity on the affected side is uniform and dense, the lack of inflatable lung tissue and the traces of bronchogram and vascular texture in it, the heart and mediastinal structure are moved to the affected side, the transverse diaphragm surface of the affected side is not clearly displayed, and the normal lung on the opposite side shows different degrees of compensatory emphysema, so that the diaphragm decreases, the diaphragm is flattened, and the over-inflated lung can form a mediastinal hernia. If you see a hemivertebral deformity of the spine at the same time, it is very helpful to diagnose. (2) Lung hypoplasia on one side: poor inflation of lung tissue on the affected side or uniform dense shadow, mediastinal displacement to the affected side, and increased brightness of lung field permeability can be seen on the healthy side. Bronchography shows a small number of bronchial branches on the affected side, a small diameter, and cystic dilation at the end. (3) Lobe hypoplasia: lung volume reduction, high density, adjacent lung field out of modern compensatory emphysema. Bronchography shows small or occlusive bronchi in the lobe, and bronchocystic or columnar dilation may be seen.
CT: (1) One side of the lung is not developed: there is no inflated lung tissue in the chest cavity of the affected side, as well as bronchogram and blood vessel texture, and the healthy side of the lung is different degrees of compensatory emphysema convex to the affected side, forming a mediastinal hernia. CT scan may reveal absent pulmonary artery on the affected side. (2) Pulmonary hypoplasia on one side: poor inflation of lung tissue on the affected side, small main bronchi, small pulmonary artery on the affected side can be seen on enhanced scanning, and sometimes abnormal venous return can be seen. (3) Lobe hypoplasia: the lung is reduced in volume, high density, triangular or circular soft tissue density shadow, usually located on the mediastinal surface of the lung, the tip of the lesion points to the lung hilar, and multiple cystic structures of different sizes and morphologies are seen in the enhanced scanning lesion.
Neonatal pulmonary hyaluronic membrane disease
Neonatal hyaline membrane disease (NHMD)
Brief history: male, 10 hours, dyspnea with decreased activity for 3 hours.
As seen in the image
Orthostatic thoracic film shows that the size and morphology of the thoracic cage are normal, bilateral symmetry, and there is no abnormality in the bone mass constituting the thoracic cage
The brightness of the two lungs is reduced, the texture of the two lungs is lost, and a large piece of ground glass density is seen in the double lungs, and the bronchogram of inflatable dilation is faintly visible inside the lungs, and the heart margin, bisphragm surface and bilateral ribophrenic angles disappear.
Preliminary diagnosis of imaging: double lung changes consider neonatal hyaluronic membrane disease
Neonatal pulmonary hyaluronic membrane disease, also known as neonatal respiratory distress syndrome (NRDS), indicates that progressive dyspnea, bruising, expiratory moaning, inhalation triple concave signs, and respiratory failure occur shortly after birth, which is one of the leading causes of neonatal death. The disease is mainly seen in preterm infants, curettage infants, or a history of asphyxia, maternal diabetes mellitus, gestational hypertension syndrome, etc. Its onset is closely related to the absence of alveolar surfactant.
NHMD pathology is characterized by high congestion, atrophy, purple-red, tough liver-like lung tissue. Microscopic results show that the lung tissue is generalized reabsorbative atelectasis, most of the alveoli and alveolar tubes are different degrees of atrophy, the alveoli walls are close to each other, the lungs only have dilated alveolar tubes and bronchiol, and their walls are attached to a uniform and structureless eosinophilic substance, that is, a transparent membrane.
Due to the many complications, rapid progression and high mortality rate of this disease, it is necessary to correctly diagnose it as soon as possible.
Radiographic manifestations of neonatal hyaluronic membrane disease of the lungs are:
(1) Polished glass shadow: due to alveolar atrophy, alveolar septum and plasma protein-rich fluid filling in the air cavity, the air cavity inflation is reduced, the lung structure is deformed and the interval is thickened, resulting in increased lung density, when the alveoli is not completely filled or completely collapsed by the liquid, the lung density is only slightly increased and the performance is ground glass shadow, which is the main sign of the disease.
(2) Tiny nodules, small nodules, acinar nodules: Due to the collapse of the alveolar cavity, primary lobules, acinar vesicles or the complete filling of fluid, the lung density of the alveolar cavity, primary lobules, and acinar levels can be increased and manifested as nodular shadows of corresponding size, and the thickening of the homogeneous mass is manifested as tiny nodules on its axial image, mainly distributed in the peripheral part of the lung.
(3) Fine reticulum nodular shadow: it is because the plasma protein-rich fluid in the alveolar septum and the fibrous transparent membrane on the alveolar wall thicken the alveolar septum, and when these thickened interstitials are present in the ground glass shadow and are not covered by solid or collapsed lung tissue, they are manifested as fine reticular nodule shadow, thus also reflecting the degree of mild to moderate damage to the lungs.
(4) Patchy, flaky, large-scale shadow: Patchy, flaky, large-scale shadow, and even "white lung" changes can be seen, and distributed according to the lobe lung segment, reflecting the collapse of the alveoli and/or the complete filling of alveoli rich in plasma proteins, occurring at the lobules, subsections, lung segments, lobes, and even the entire lung level.
(5) Bronchiectasis: bronchodilation can be seen in the periphery of the lungs or terminal bronchiolecta below bronchiecta, showing short-pointed fine or short bald dendritic branches, CT appears as vesicle-like and irregularly dilated bronchogram, because the atrophy of the alveoli or being filled by liquid is the body's gas exchange function is reduced, in order to maintain normal gas exchange, the small airway with gas exchange function compensatory hyperinflation, so passive dilation. Therefore, most scholars consider inflatable bronchial signs to be characteristic radiographic signs of the disease. Bronchiectasis that occurs simultaneously at the lobular level can also be seen in lung diseases such as lobular pneumonia, connective tissue lung disease, nonspecific interstitial pneumonia, and viral pneumonia.
Congenital cystic adenomatous malformations
Brief medical history: male, 1 year and 4 months, repeated cough, sputum cough for more than 1 month
Images: Figures A and C: Reconstructed lung window for CT sweep axis position and coronal position, showing that the left thoracic cage is smaller than the contralateral side, and the right lower lung sees multiple cysts of different sizes without lung texture translucent shadows, similar to honeycomb changes, and the intercystics are irregular thickness and thickness of unequal density increased shadows. Figures B and D: Reconstruct the mediastinal window for CT sweeping the axis position and coronary position, showing that part of the space in the right lower lung lesion area is soft tissue density shadow.
Preliminary diagnosis of imaging: multiple cystic translucent images of the right lower lung, considered congenital cystic adenoma-like malformations.
Congenital cystic adenomatoid malformation (CCAM) is a 7 to 10 weeks of embryonic stagnation due to unknown factors affected by unknown factors in the development of fetal lung buds, alveoli do not develop and caused a large proliferation of pulmonary interstitium, forming a clump of disorganized lung tissue that communicates with normal bronchi and has separate blood supply arteries and drainage veins. According to the pathological histology, it is divided into 3 types: (1) type I (large cyst type): there is a large thick-walled cyst cavity with a diameter of >2 cm, and there may be a small cystic cavity around it; The cystic cavity is lined with pseudo-laminated ciliated columnar epithelium, smooth muscles and elastic fibers may be around the sac wall, and there are alveolar structures between or adjacent large cysts of the large sac. (2) Type II( multiple small cyst type): the lesion is dominated by multiple separated cyst cavities, the maximum cystic cavity diameter is more than l cm, the cyst is lined with cubic or high columnar ciliary epithelium, and rarely is pseudo-compound epithelium. (3) Type III. (substantial mass type): the lesion is generally similar to a lung tissue mass, and is mainly manifested as a solid mass,
There is no cystic cavity that is distinguishable to the naked eye.
There are three main imaging manifestations based on its pathological typing: (1) macrocystic type: there can be two manifestations, one is a pneumothorax-like change on x-ray plain, and a single pneumothorax that occupies most of the chest cavity; The other is x-rays showing multiple cystic changes of varying sizes. (2) Small cyst type: it is manifested as a multi-like honeycomb small cyst-like change of similar size, most of which is a thin-walled air-containing cyst cavity, and the sac wall is thickened when infection occurs. (3) Solid type: it is manifested as a change similar to lung mass and atelectasis, and X-ray is manifested as multiple dense solid deformation of double lower lung.
Lung odd lobes
Brief medical history male, 47 years old, complaint of no discomfort, routine physical examination.
Image: Figure A ~ E: Figure A, Figure B Lung Window and Figure E Lung Window Three-dimensional Reconstruction Image. Figures C and D mediastinal window sweep and arterial phase images can show that the odd vein with walking variation can be seen in the upper lobe of the right lung, which is integrated into the superior vena cava at a higher position, and the medial part of the upper lobe of the right lung separated by the odd vein is the odd lobe, and above the odd vein arch, it can be shown that there is a clearly demarcated, slightly convex, slightly convex interlobar pleura between the odd lobe and the upper lobe of the right lung, which is a odd vein fissure. Fig. F : A thin linear shadow from the right lung tip inwards and down to the lung hilum on the orthostatic chest x-ray, and its end point is an inverted comma-like, which is a vertical projection of the odd fissure and odd vein section.
Preliminary diagnosis of imaging: Odd lobe malformation of the upper right lung.
Pulmonary azygos lobe is a rare type of lung anatomical variant that is more common in men than in women. Odd lobes occur on the mediastinal side of the upper lobe of the right lung. The root cause of the occurrence of the odd lobe of the lung is still not very clear, most scholars believe that the embryonic stage of the odd vein arch does not fall with the heart's large blood vessels in the mediastinum, but free in the lungs and together with the pleura downward caused, at this time the odd vein together with the pleura in the lobe of the lung to form a deep incision, called odd vein cleft.
Since the odd vein is located outside the parietal pleura, the odd vein fissure is composed of two parietal layers and two visceral layers of pleura. The medial portion of the upper lobe of the right lung is separated from the upper lobe of the right lung by the pleura and is called the odd lobe due to its abnormal location, and its blood supply comes from the posterior segment of the apex of the upper lobe of the right lung.
On orthostatic chest x-ray, a curved, thin cord-like shadow can be seen, starting at the inner edge of the clavicle at the right apical apex, and a small triangular pointed protrusion can be shown at the pleural fold at the beginning of the right lung tip, which runs inward from the tip of the lung to above the hilar, ending at the root of the right lung, showing an inverted comma shadow (or "teardrop shadow"), which is a vertical projection of the odd vein section.
Typical CT images can show the odd veins with walking variations, which are fed into the superior vena cava at a higher position, and the odd lobes and odd lobes formed by the compression of the pleura by the odd veins, the odd fissures present a thin arc-like shadow with a continuous multilayer clear boundary and slightly convex outwards, extending from the side of the spine to the anterior chest wall, and the triangular air-containing tissue formed by the odd fissures and vertebral bodies and mediastinum is the odd lobes.
In clinical practice, it should be noted that sometimes similarly positioned cordoid shadows can be misdiagnosed as odd lobes, such as scars, large vellicular walls, pleural adhesions, pleural depressions, etc., but CT images can show odd veins in normal positions and can detect underlying diseases, which can be identified.
The pulmonary lobes themselves have no pathological significance, do not cause clinical symptoms, and do not require treatment if there are no other comorbidities. The clinical significance of the chiloe is mainly: (1) If the odd vein compresses the bronchi that supplies the odd leaf, it can cause the chi leaf to develop atelectasis or bronchiectasis; (2) The occurrence of odd lobe parafiss, odd lobe parafiss is different from other interlobaular fissures, odd lobe parafiss are high, and it is a fissure formed by bilayer pleura, and the general pleural effusion is not easy to enter, if it enters, it is often complicated by pleurisy effusion; (3) In X-ray examination, the odd lobes of the lungs can be clearly displayed, which is of great significance for determining the surgical scope of lobectomy.
Congenital thoracic deformities (funnel chest, chicken breast)
Brief medical history: male, 5 years old, main complaint: Discovery of depressed deformity at the thoracic sphire process for more than 3 years.
Image: Figure A: Orthostatic chest X-ray showing mild left shift of the cardiac shadow, pulmonary artery segment expansion, thoracic spine mild left convex scoliosis; Figure B: Lateral chest x-ray shows inward depression of the lower sternum and the saber process, the anterior space of the heart is significantly reduced, and the distance between the posterior sternal edge and the anterior edge of the spine is reduced. FigureS C to F: Ct mediastinal window cross-section and sagittal reconstruction show that the lower sternum is depressed towards the spine, the thorax is funnel-shaped, and the poststernal heart is pressurized and shifted to the left.
Initial diagnosis of imaging: congenital funnel chest.
Congenital wall deformities are congenital developmental disorders of the chest wall, causing some chest wall shape and anatomical abnormalities, including funnel chest, chicken breast, Paland syndrome, and sternal fissure. Other skeletal disorders can also cause chest wall deformities, which are local changes in the chest of systemic diseases.
1. The pectus excavatum or funnel chest is the most common type of chest wall deformity, accounting for more than 90% of chest wall deformities, and the incidence can reach 0.1% to 0.3%. The infundola is a congenital disease that can be accompanied by other congenital malformations, the onset of which is not related to "calcium deficiency", 10% to 20% of children have a clear family history, more male than female, about 4: 1,90% are found within 1 year of birth, generally worsened with the growth and development of the child. The specific cause of the funnel chest is still not fully understood. The funnel thorax is characterized by a depression in the lower part of the sternum and its corresponding rib cartilage in the direction of the spine, forming a funnel-shaped depression of the anterior chest wall centered on the sword process. The clinical manifestations of the funnel chest vary with the degree of chest wall deformity, the degree of deformity is mild, there is no heart and lung function damage, and often no other symptoms, but with the worsening of the degree of deformity, typical funnel chest signs appear: "shoulder forward leaning, back arching, anterior chest wall depression, abdominal bulge", severe cases can affect the child's respiratory and circulatory function. Funnel thoracic deformities can be symmetrical or asymmetrical. Funnel-thoracic deformity in young children
It is often symmetrical, asymmetrical with age, accompanied by sternal rotation, and some scoliosis and other secondary deformities. Chest x-ray or CT can help determine the extent of chest wall deformities and the presence or absence of comorbid deformities.
2. Chicken breast (pectus carinatum) accounts for about 6% of chest wall deformities, male: female incidence is about 3:1, generally more common in older children and adolescents. Contrary to the funnel chest, in general, the incidence of chicken breast is mostly related to calcium and phosphorus metabolism, but it is also clinically found that there are patients with funnel chest and chicken breast coexisting in the family. Chicken breasts generally have no other manifestations except for the appearance of chest wall deformities, but the presence of deformities can cause psychological burdens, and patients with severe deformities can also have clinical manifestations of heart and lung insufficiency due to heart and lung compression. Chicken breast is mainly characterized by a convex deformity of the anterior thorax wall, most cases are symmetrical anterior protrusion of the sternum body and the inferior rib cartilage connected to it, a few asymmetrical deformities with unilateral bulges, a few cases are mixed deformities, one side is raised and the other side is concave, or the upper segment is a chicken breast and the lower end is a funnel thorax change, but the sternum stalk and the associated rib cartilage are convex and the sternum body is less common. Chicken breasts can often be accompanied by valgus of the ribbed margin, and in severe cases, scoliosis can also be secondary.
Straight back syndrome
Brief history: male, 14 years, anemia.
Image view: Figure A: Chest orthostatic film showing bilateral symmetry of the thoracic cage, clear texture of both lungs, no obvious abnormal density shadow in the field of both lungs, the heart is mitral valve type, and the pulmonary artery segment is slightly protruding. Fig. B : Lateral thoracic vertebrae show that the physiological curvature of the thoracic spine is absent, the anteroposterior diameter of the thoracic cage is narrowed, and the ratio of thoracic transverse diameter to sagittal diameter is about 2.8.
Initial diagnosis of imaging: thoracic changes, in combination with clinical practice to exclude straight-back syndrome.
Straight back syndrome (SBS) is also known as flat chest syndrome. Due to the disappearance of physiological curvature of the thoracic spine, the anterior and posterior diameter of the thoracic cage narrows, placing the heart between the narrow sternum and the thoracic spine, resulting in a series of symptoms. Rawlings calls it "pseudo-heart disease." Patients may hear grades 1 to 4 systolic murmurs with hyperparagraphy in the left sternal margin between the ribs 2 to 3. Some patients have symptoms such as post-activity palpitation, chest tightness, dizziness, fatigue, etc., and some have no self-conscious symptoms. The cardiac murmur is produced due to the narrowing of the anterior and posterior diameter of the thoracic cage, so that the right ventricular outflow tract is close to the anterior chest wall, so that the normal physiological ejection sound is easy to conduct. At this time, ECG and echocardiogram are mostly normal. Chest x-rays are an important basis for diagnosing anthoposynes syndrome. On the orthostatic chest x-ray, there was no obvious change in the blood of the two lungs, the heart shadow was mitral valve type, the pulmonary artery segment was slightly convex or straight, and the cardiothoracic ratio was generally larger. Sagittal radial thoracic altruism can be seen on lateral chest x-ray, especially in the 8th thoracic vertebral plane, with the outflow tract clinging to the anterior chest wall. When the ratio of thoracic diameter to sagittal diameter is greater than 2.5, the possibility of straight back syndrome should be considered. The thoracic transverse diameter refers to the widest diameter of the inner edge of the thoracic cage horizontally at the apex of the right diaphragm. The sagittal diameter is the diameter between the anterior middle of the 8th thoracic vertebral body and the posterior sternum margin (2 mm minus in adults and 1 mm in children, as the thickness of soft tissues in the inner wall of the chest).
In summary, when diagnosing anthoposyl syndrome, straight back (flat chest) and clear murmurs at the base of the heart are two necessary conditions, and the presence of organic heart disease (such as atrial septal defects, pulmonary stenosis, idiopathic pulmonary artery dilation, etc.) should be ruled out first, and then the disease can be considered.
Source: Image Time
【Copyright Notice】This platform is a public welfare learning platform, reprinted for the purpose of transmitting more learning information, and has indicated the author and source, such as teachers who do not want to be disseminated can contact us to delete