Behind the increasing westernization of diets and the increasing number of obese people is the current situation that the detection rate of reflux esophagitis (RE) is increasing year by year1. However, in the face of rees with explosive combat effectiveness, how should we fight this battle?
Currently, proton pump inhibitors (PPIs) and novel potassium ion competitive acid blockers (P-CAB) are both acid-suppressing drugs for the treatment of RE.
P-CAB's representative drug fumarate funolasine tablets (referred to as "vonorasin") has been confirmed by a number of clinical studies with good acid inhibition efficacy and safety. A Japanese phase III clinical study of Vonorasin showed that the healing rate of THE RE mucosa at 4 weeks of Vonorasin was comparable to that of Lansoprazole at 8 weeks, 96.6% and 95.5%, respectively. Another network meta-analysis confirmed that for patients with all levels of RE, a shorter course of vonorasin (4 weeks) was comparable to a standard course of PPIs (8 weeks).
However, after the initial treatment, is it possible to "sit back and relax"?
First, let's first understand the World Health Organization's (WHO) definition of chronic disease4, which refers to "a slower-developing long-term disease", which has three elements: chronic, progressive, and complications.
However, RE has chronic characteristics that are difficult to cure and easy to recur, and the condition often fluctuates during treatment. Data from a set of placebo-controlled trials showed 5 that after at least 6 months of maintenance therapy, the average recurrence rate of esophagitis in patients receiving placebo was 75%, and the average recurrence rate of esophagitis in patients receiving PPI was 28%. Without maintenance therapy after initial PPI treatment, the recurrence rate of symptoms in PATIENTS with RE within 6 months of discontinuation is as high as 90%. Relapse can significantly affect patients' quality of life6, and compared with patients without recurrence, patients with relapse have decreased sleep quality and increased scores for depression and anxiety.
RE is a progressive disease in which a certain percentage of patients progress from non-erosive esophagitis (NERD) to Barrett's esophagus (BE) and are at risk of progressing from mild RE to severe RE (10% to 22%), and finally to BE7-8. In addition, over the past 30 years, RE has become one of the causes of severe upper gastrointestinal bleeding9, bringing the latter from 1.6% to 7.7%. 64% of PATIENTS with severe upper gastrointestinal bleeding did not take acid-suppressing drugs before the bleeding occurred, and did not undergo long-term effective management.
At the same time, persistent/untreated chronic esophageal acid exposure can lead to changes in the anatomy and structure of the esophagus10, which can lead to a variety of complications such as esophageal ulcers, esophageal stenosis, esophageal bleeding, BE, and even esophageal adenocarcinoma.
At present, it is widely believed that the pathogenesis of BE begins with chronic esophageal injury caused by GERD. Existing studies have linked 11,BE to transdifferentiation and transcommitment; cell studies of their origin have also been discussed, including squamous epithelial basal cells, esophageal submucosal gland cells and their ductal cells (ESMGs), proximal gastric cells, special cell populations at the gastroesophageal junction, and circulating bone marrow cells (Figure 1).
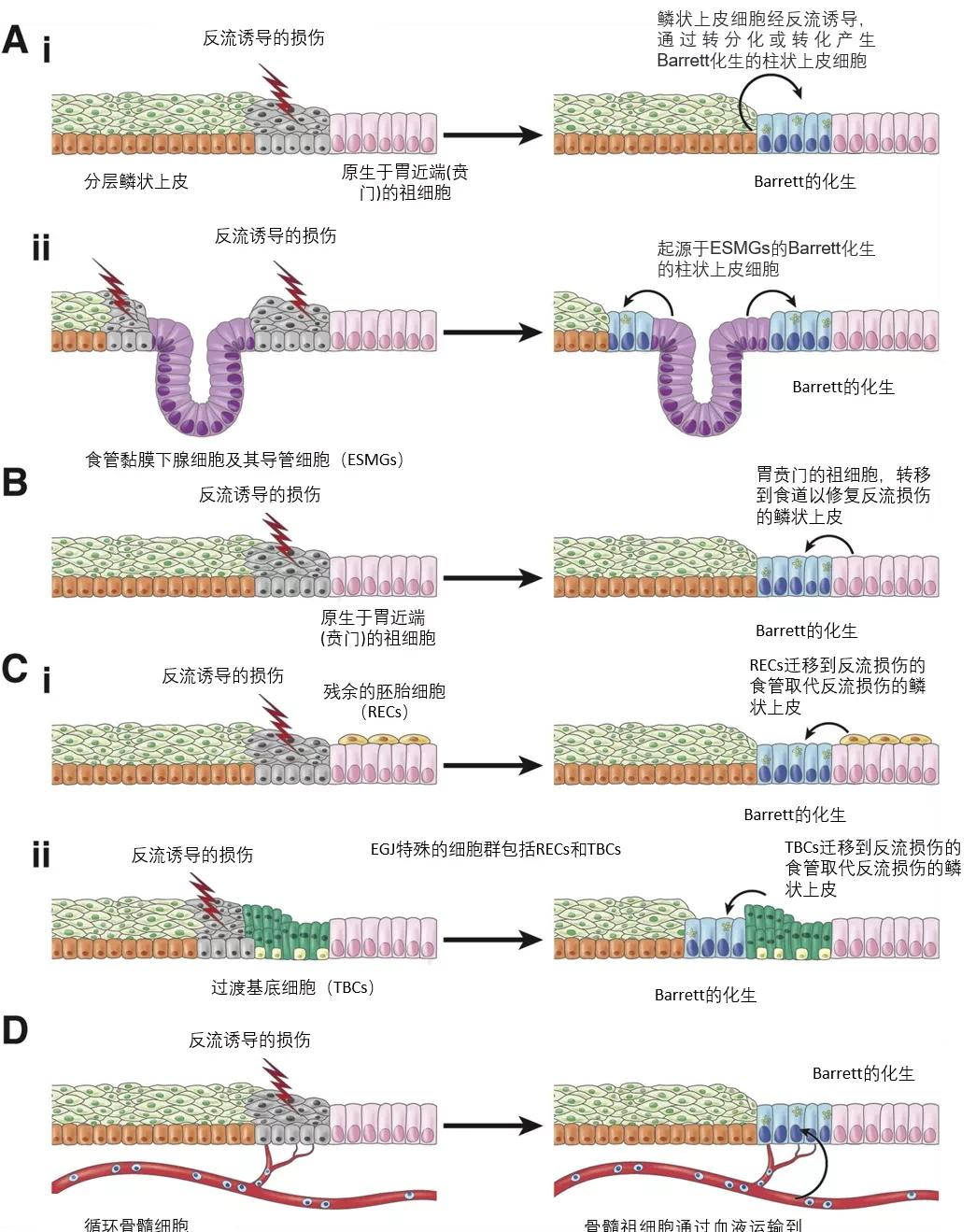
Figure 1 4 types of origin cells of BE
Therefore, having an initial treatment alone is not enough for RE!
The 2013 American Society of Gastroenterology GERD Diagnosis and Treatment Guidelines, the 2015 Japanese Society of Gastroenterology GERD Evidence-Based Clinical Practice Guidelines, the 2017 World Gastroenterology Organization (WGO) Global Guidelines, and the 2020 Chinese Medical Association Gastroenterology Branch China GERD Expert Consensus all recommend 12-15, RE is a progressive chronic disease that requires initiation therapy + maintenance therapy to continuously relieve symptoms and maintain mucosal healing.
So, which maintenance treatment is better?
Lifestyle changes are fundamental to the management of RE throughout the process, including: weight loss, smoking and alcohol cessation, avoiding night food, raising the head of the bed, and stopping chocolate, caffeine, spicy and other foods12. In terms of drug therapy, the initial course of treatment for P-CAB and PPI for RE was 4 weeks and 8 weeks 2-3, respectively.
However, there are differing opinions among physicians regarding the choice of maintenance treatment strategy. Survey results of a questionnaire survey of 585 medical professionals (221 gastroenterologists, 205 primary care physicians, 159 otolaryngologists) from 7 countries and regions in Asia Pacific showed that 16,54% of gastroenterologists preferred long-term maintenance therapy, 38% preferred on-demand treatment, and 9% chose intermittent therapy.
One systematic review17, including 14 studies, systematically evaluated the efficacy of histamine H2 receptor antagonists or PPIs on intermittent and on-demand treatment in patients with RE or symptomatic heartburn. The results confirmed that symptom-driven, on-demand treatment regimens were more appropriate for patients with NERD.
For patients of LA A-B grade, studies showed 18, with on-demand therapy for 20 weeks after 8 weeks of initial treatment, with nearly 60% recurrence of symptoms and nearly 60% of mucosal non-healing rates. Patients with RE who underwent long-term maintenance therapy 24 weeks after 19 weeks had better mucosal healing than those who opted for on-demand therapy. Patients with RE who underwent long-term maintenance therapy 20 months later, and the number of patients who maintained the healing state of the mucosa was greater than those who received on-demand therapy. After 6 months of long-term maintenance therapy, patients with RE had a lower recurrence rate than those who received on-demand therapy.
The 2020 AMERICAN JAMA JOURNAL GERD review further states that 21: Patients with RE should opt for low-dose once-daily maintenance therapy. Patients with esophagitis and BE, even when no symptoms occur, should receive a low dose of once-daily PPI to reduce the risk of esophagitis recurrence or tumors.
Scratch the point!
AS A chronic disease with complex etiology and easy recurrence, persistent mucosal damage has an increased risk of other complications;
Guidelines and consensus on the management of RE have been clarified, and patients need to be managed throughout the process;
No maintenance therapy is a risk factor for RE recurrence, and maintenance therapy can reduce the risk of RE recurrence;
Patients with RE should be selected for once-daily maintenance therapy.