Nine institutions jointly issued a consensus on home medication for children's respiratory tract infections
Interviewee: Zhang Silai, former director of the Department of Pediatrics, Hospital of Integrated Traditional Chinese and Western Medicine, Beijing University of Chinese Medicine
Global Times health client reporter Zhong Caifen
This winter, respiratory infections are on the rise, and pediatric clinics across the country are overcrowded. For the vast majority of patients, home medication is an important part of disease treatment. In order to improve the level of home medication management for children's respiratory tract infections, nine professional institutions, including the Pediatric Professional Committee of the China Medical Education Association and the Asthma Collaboration Group of the Respiratory Group of the Pediatric Branch of the Chinese Medical Association, jointly issued the Expert Consensus on Home Drug Medication Guidance for Children with Respiratory Tract Infections (hereinafter referred to as the "Consensus"), giving advice and guidance on many medication issues that parents are concerned about. To this end, the "Global Times Health Client" specially invited Zhang Silai, a well-known parenting expert and former director of the Department of Pediatrics of the Hospital of Integrated Traditional Chinese and Western Medicine Affiliated to Beijing University of Chinese Medicine, to interpret the main content of the "Consensus".
1. What are the common symptoms of respiratory tract infections in children?
The consensus concludes that respiratory tract infections in children can be divided into upper respiratory tract infections and lower respiratory tract infections according to the location of infection. Upper respiratory tract infections mainly include the common cold, influenza, pharyngitis, etc. Lower respiratory tract infections mainly include bronchitis, pneumonia, etc. Zhang Silai said that if the child has one of the following conditions during the influenza epidemic period, it is necessary to have a high suspicion of influenza infection: sudden onset, accompanied by acute respiratory symptoms such as fever, cough or sore throat, and continue to worsen within a few days; in addition to fever, headache, body aches, infants and young children show listlessness or abnormal irritability, poor appetite, etc.; infants and young children have sudden fever, oral antipyretic drugs body temperature drop is not obvious, and there is a continuous state of high fever.
2. What should I pay attention to when taking medication for respiratory tract infections in children?
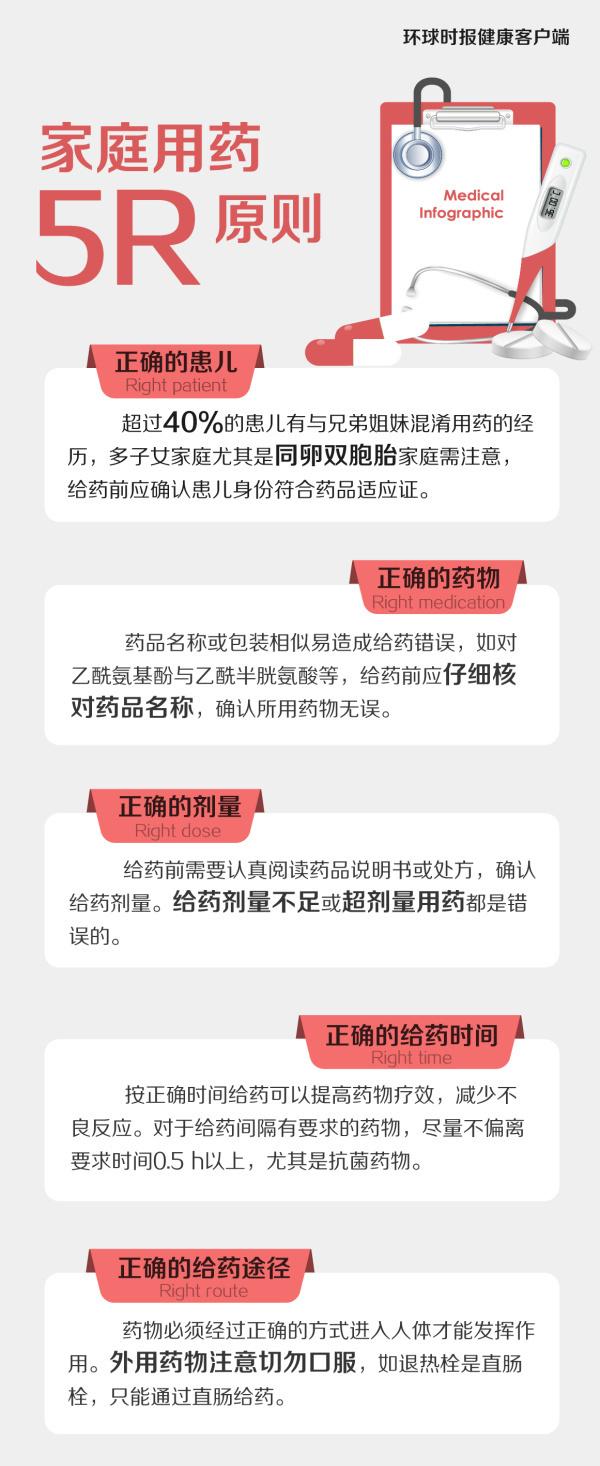
The "Consensus" reminds that home medication needs to follow the 5R principle, namely: the right child, the right drug, the right dose, the right time of administration, and the right route of administration.
3. Do children with respiratory tract infections have to use antimicrobial drugs?
The Consensus reminds that there are many causes of respiratory tract infections in children, and if it is a simple viral infection, antimicrobial drugs are ineffective, and antimicrobial drugs should be used as appropriate when bacterial infections are combined or secondary. In addition, antimicrobial drugs are prescription drugs and must be used after comprehensive evaluation by a physician. Zhang Silai said that the current trend of infusion and antimicrobial application is proliferating, which may lead to the development of drug resistance of pathogens, which is not conducive to maintaining children's long-term health.
4. When should antivirals be used?
There are many viruses that cause respiratory infections in children, and there are no specific antiviral drugs for viruses other than influenza virus and cytomegalovirus. Zhang Silai introduced that at present, for the influenza virus, the more effective drug is oseltamivir, which is only for the influenza virus, and is ineffective against the common cold, herpes virus, Epstein-Barr virus, coronavirus, adenovirus, rhinovirus, etc. Taking it within 48 hours of the onset of illness can help control the condition, shorten the course of the disease, and prevent complications.
5. When should antipyretic analgesics (antipyretics) be used?
Antipyretic analgesics may be used ≥ 2-month-old infants with an axillary temperature of ≥ 38.2 °C or significant discomfort and mood changes due to fever. At present, there is no comfort scale specifically for children with fever, and it is recommended to use the internationally accepted Wong-Baker Facial Expression Pain Scale (see figure below) to assess the comfort level of children with fever.
According to Zhang Silai, there are generally two types of antipyretics suitable for children, namely acetaminophen (Tylenolin) and ibuprofen (Motrin). Among them, acetaminophen is safer and is the first choice for babies over 3 months old, and ibuprofen is more suitable for children over 6 months old or with acetaminophen that does not have a good antipyretic effect. The specific dosage should be determined after a comprehensive assessment of the child's age and weight, and the two drugs should not be used interchangeably, nor should they be used at the same time with compound cold medicines containing antipyretic and analgesic ingredients. Oral formulations such as drops or suspensions are preferred for children, drops of high concentration and small volume are preferred for younger children (eg, under 3 years of age), and acetaminophen is preferred for gastrointestinal discomfort and fever.
6. What should I do if my child still has a fever after taking medication?
Generally speaking, the child's body temperature will gradually drop after the disease is relieved, and parents should not increase the frequency or dose of off-label administration due to anxiety, so as not to cause harm to the child. If there are still fever symptoms after taking the drug, parents can check whether the drug is used correctly to ensure that the drug has not exceeded the expiration date, the suspension is shaken well before use, and the dosage is accurate. At the same time, the medication can be combined with appropriate physical methods to cool down, such as antipyretic patches, warm water external application and warm water baths. Zhang Silai reminded that it is best for children to drink a small amount of water after taking antipyretics, so as to speed up the excretion process and help to take away the body heat; when the fever exceeds 38.5 °C, antipyretics are the first choice, followed by physical cooling; if the fever is high and persistent, it is necessary to see a doctor.
7. Should I use cough suppressants when I have a cough?
Cough is a protective reflex to clear respiratory secretions or inhaled material, and cough following a respiratory infection in children may persist for several weeks after the resolution of symptoms of other infections and gradually resolve without intervention, with 50% of children having cough associated with an upper respiratory tract infection resolving within 10 days. The consensus does not recommend the routine use of antitussive drugs, and the use of antitussive drugs can be considered for symptomatic treatment when the cough significantly affects the child's sleep and diet.
8. What should I do if my child has phlegm?
The use of expectorants or phlegm-reducing drugs should first identify the cause of sputum cough and select drugs according to the characteristics of sputum. The "Consensus" reminds that children with rare hereditary fructose intolerance symptoms should not take oral preparations containing sorbitol, and children with asthma are prohibited from taking oral acetylcysteine, and nebulized acetylcysteine should be used with caution. Zhang Silai said that the production of sputum after infection is the body's self-protection mechanism, and when the sputum is excreted from the body, it will also expel the dust, bacteria, viruses, and necrotic cells that adhere to it. At present, there is no evidence in clinical studies that children with respiratory tract infections can benefit from taking expectorant drugs, so it is not recommended to give expectorant drugs to children with phlegm easily.
In the absence of medication, the "Expert Consensus on the Management of Airway Mucus Hypersecretion in Children" mentions two physical expectorant methods suitable for home application: one is chest percussion. Helping your child tap the chest wall near the sputum from the bottom up and from the outside to the inside will make it easier for the sputum to fall off the tube wall. Percussion is suitable for waking up in the morning, 30 minutes before meals or 2 hours after meals, and it is advisable to do 3~10 minutes each time. The second is cough training. It is recommended to take a sitting cough to discharge sputum, first take 5~6 deep and slow breaths, then inhale deeply until the diaphragm is completely lowered, hold your breath for 3~5 seconds, lean forward, and make 2~3 short and powerful coughs from the chest, or press the upper abdomen with your hands to help the phlegm cough out.
9. Which respiratory infections can be nebulized?
According to the Consensus, the indications of nebulized inhalation therapy in children with respiratory tract infectious diseases include the following types: (1) acute laryngitis, acute laryngotracheobronchitis, acute epiglottitis, whooping cough or pertussion-like syndrome, pneumonia, etc.; (2) infant wheezing including bronchiolitis, wheezing bronchitis, etc.; (3) others such as cough after respiratory tract infection, obliterans, etc.
Home atomization can save parents' time and transportation costs, avoid cross-infection in hospitals, and make up for the lack of medical resources. The "Consensus" reminds that it is necessary to seek medical guidance before home atomization, and it should be noted that the nebulized drug cannot be stored in the nebulizer for a long time, and the dosage of each nebulization is 3~4 ml is advisable to avoid excessive nebulization time affecting children's compliance; avoid excessive eating 30 minutes before nebulization; do not apply oily creams before the use of hormone drugs; children should best carry out nebulization inhalation treatment in a sitting quiet state, infants and young children can take a semi-sitting and lying position; clean the face in time after the nebulization, rinse the mouth with water 3 times or more, and use cotton swabs to wipe the mouth for nursing care for small babies.
10.Can children with respiratory tract infections use proprietary Chinese medicine or Chinese medicine?
According to the syndrome type, the commonly used Chinese patent medicines for respiratory tract infections can be divided into clearing heat and detoxifying, clearing the lungs and dissolving phlegm, relieving the surface of spicy and warm disease, relieving the surface of spicy coolness, dissipating wind and cold, relieving fever and relieving pain, clearing heat and relieving the surface, relieving pharyngeal swelling, relieving cough and expectorant, calming the nerves and eliminating accumulation, etc. Zhang Silai emphasized that Chinese patent medicine or traditional Chinese medicine should be used rationally after asking a physician to distinguish between syndromes and diseases, or after combining syndrome differentiation and disease differentiation. At the same time, it is necessary to carefully understand the ingredients of the drug and avoid the combined use of proprietary Chinese medicines with the same function or duplicate ingredients. Priority is given to children's drugs with words such as "children", "children" and "dolls" in their names.
11. What should I do if I have a stuffy nose?
Nasal congestion can interfere with children's water intake and sleep, and is one of the most troubling symptoms. According to the Consensus, when nasal congestion symptoms occur, normal saline can be used to clean the nasal cavity, and nasal decongestants can be used for a short time under the guidance of a physician if the cleaning effect is poor. Commonly used nasal decongestants include oxymetazoline (contraindicated in children under 2 years of age) and xylozoline 0.05% (not recommended for children under 3 years of age). Nasal decongestants should not be used for more than 7 days to avoid causing drug-induced rhinitis. Patients with atrophic rhinitis and dry nasal cavity are prohibited.
12. What should I do if my child can't be fed medicine?
The "Consensus" proposes that special attention should be paid to children's emotions and comfort, and that they should be provided with a safe, warm and comfortable environment and way as much as possible. You can choose to use some professional feeding aids, such as measuring cups, droppers, pacifiers, etc. For infants, do not pinch the nose to fill the medicine, it is best to hold the semi-recumbent position in the arms of the adult, pinch the chin so that the mouth is open, and then use a dropper or needle feeder to feed the medicine in small quantities and many times. Wait for your child to swallow before continuing to administer the medicine, and stop choking immediately. Children over 1 year of age can be encouraged to take the drug by giving appropriate incentives.
13. Can I use juice or milk to deliver medicine?
Some parents may feel that their children are not easy to reject the medicine with juice or milk, but the "Consensus" reminds that juice or milk may affect the absorption and efficacy of the drug in the gastrointestinal tract, and it is best to use plain water at the right temperature to take the medicine.
14. Do I need to take up the medicine if I vomit after taking the medicine?
Vomiting after taking the drug is common in children. According to the "Consensus", whether supplementary medication is needed should be analyzed according to the characteristics of drug absorption and metabolism, the time and situation of vomiting. If you vomit immediately after taking the drug, and the vomit is seen in the complete tablet, capsule, or all of the liquid, you may consider taking a catch-up dose. If you take it for more than 15 minutes, you need to weigh the potential risk of missing a dose and the harm of overdose after a top-up dose before deciding whether to take it again.
15. How to store home medication?
The "Consensus" suggests that it should be stored in accordance with the specific requirements under the drug instructions [storage], cold place usually refers to 2~10 °C, cool refers to no more than 20 °C, cool implicit refers to no more than 20 °C and away from light, and the room temperature is 10~30 °C. Attention should be paid to the storage of medicines: separate from food, beverages, cosmetics, etc., and keep them out of reach of children; tighten the bottle cap after medication, regularly check the expiration date and quality of drugs, and clean up in time if there is any deterioration such as expiration and change in character.
Zhang Silai finally reminded that under normal circumstances, the treatment of children's respiratory tract infections should follow the principle of "no medicine if you can do without medicine, no injection if you can take oral medicine, and no infusion if you can get an injection". In mild cases, home care is prioritized to avoid cross-infection caused by going to the hospital. If symptoms such as fever persist for 3 days after intervention in the correct way, medical attention should be considered. ▲
Editor-in-charge: Pan Zihu
Editor-in-Chief: Ding Wenjun