<h1 class="pgc-h-arrow-right" data-track="1" > organs in the small pelvis include the colorectum, bladder, urethra, uterus, fallopian tubes, ovaries, and vagina. </h1>
The pelvic colon is surrounded by peritoneum and is connected through the mesenteric membrane to the midline of the left psoas major muscle and the sacrum, down to the third sacral vertebrae.
The rectum begins in the third sacral vertebra and extends downwards to the tip of the coccyx. The upper 1/3 of the front and sides are covered with peritoneum, the middle 1/3 is covered by the peritoneum in front, and the lower 1/3 is not covered by the peritoneum. During pregnancy, the space between the uterus and the sigmoid colon becomes smaller, causing or worsening constipation.
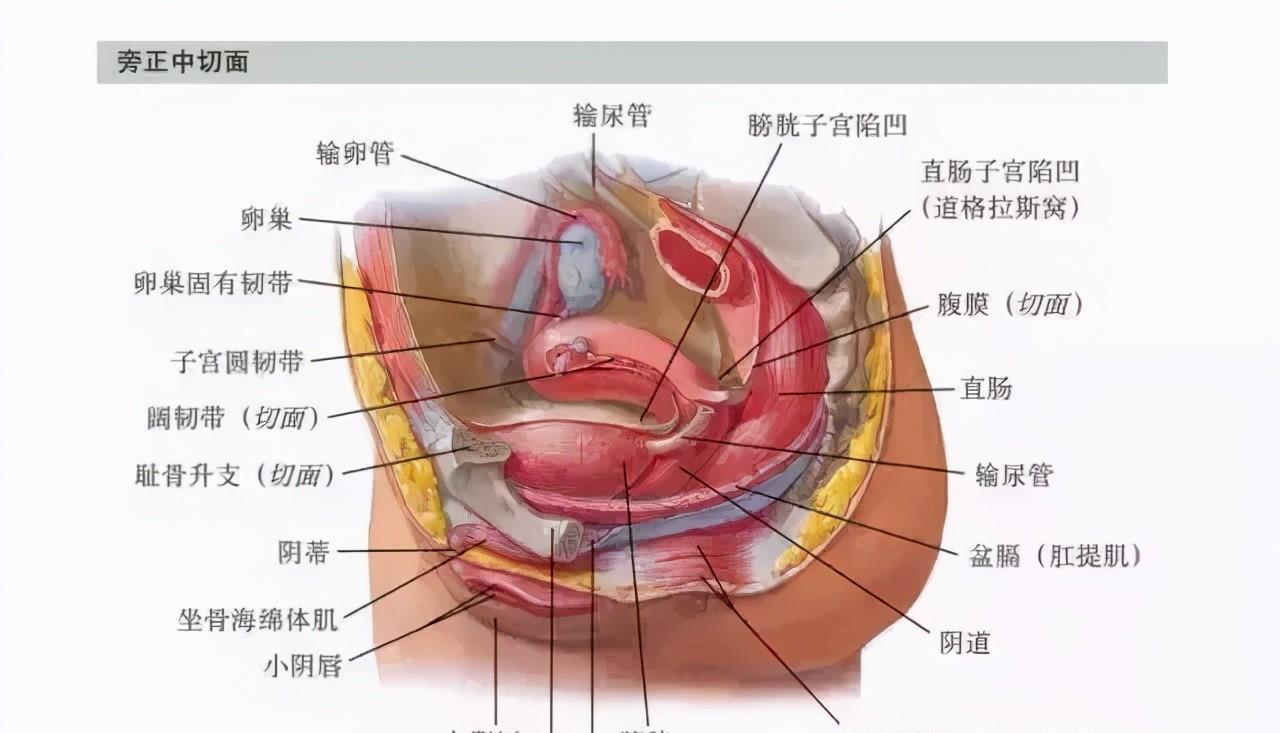
The mid-section next to the pelvis
The ureter crosses the front of the common iliac artery into the true pelvis and down the lateral pelvic wall to the pelvic floor. At the ischial spine level, the ureter travels mid-front, under the broad ligament, between the uterine artery and the vaginal artery, to the side of the vaginal dome. At this level, the ureter is approximately 2 cm from the uterus, which is where the ureter is susceptible to damage during hysterectomy.
The bladder is located behind the pubic joint, in front of the uterus and vagina. The bottom of the bladder is directly connected to the anterior vaginal wall. The bladder neck is located above the diaphragm and is connected to the urethra. The upper part of the bladder is covered by the peritoneum and is in contact with the uterine body and the uterine floor of the preflexion position. This layer of peritoneal folding is necessary to open during caesarean section. The Retzius space is located between the pubic bone and the bladder and is filled by extraperitoneal adipose tissue.
The two sectional anatomys on this page show the relationship of the uterus to the tissues around it. The upper part of the uterine floor is usually convex and forward-facing. The anterior wall of the uterus is flat and appears to lie forward and downward on the bladder. The peritoneum covered anterior to the uterus folds back in the isthmus to form a bladder uterine depression. The posterior wall of the uterus is also convex, adjacent to the colon and rectum. The posterior peritoneum covers the uterine body and the upper part of the cervix, and then extends the dome to reach the rectum to form a rectal hysteresis, also known as the Douglas fossa. The peritoneum forms the anterior and posterior lobes of the broad ligament on the lateral side of the uterus.
The cervix points down to the posterior side of the vagina. Only the upper 1/2 of the posterior cervix is covered by the peritoneum. The external cervical orifice is located on the horizontal plane of the upper border of the pubic symphyllum and on the coronal surface in the ischial spine plane.
The middle of the pelvis
Pelvic organs and their support system – viewed above
Pelvic view (peritoneal intact)
The intrapelling fascia (pseudofacia) refers to the fascia that folds back on the surface of the organs above the pelvic diaphragm. When the cavitary organs of the pelvic floor enter the pelvic cavity through the pelvic floor, the intrapelvis fascia adheres to these organs to form a collar-like tubular fibrous tissue, which is inextricably linked to the pelvic floor muscles below. Thus three tubular fascial tissues are formed at the pelvic floor, including the urethra and bladder, the vagina and the lower uterus, and the rectum. These pelvic organs have crossed muscle fibers within the fascia tissue on the surface of the organs and can be used to repair the bulging of the anterior and posterior walls of the vagina. It is also in this layer of fascia that is covered with the lower uterus, and the intrafascial hysterectomy is performed in this layer of fascia to maintain the supporting structure of the top of the vagina.
The pelvic fascia on the surface of the bladder, uterus, and rectum is connected to the fascia above the pelvic diaphragm, including the oblongata fascia, iliac fascia, and transverse fascia. Structures that directly or indirectly maintain the position of the uterus include the peritoneum, ligaments, fibrous tissue, and fibromuscular tissue. The most important of these tissues are the main ligament and the pelvic diaphragm and the intrapelvis fascia above it.
The bladder peritoneal fold and the rectum uterine peritoneal fold are often considered ligaments anterior and posterior to the uterus. But they are not true ligaments and have a limited supportive effect on the uterus. The round ligament is a flat, fibrous muscular tissue that, along with the visceral peritoneum, travels outwards and downwards from the anterior wall of the uterus to the labia majora through the inguinal canal.
Pelvic view above
The uterosacral ligament is a true muscle-fibrous ligament structure that emanates from above the cervix and travels posteriorly to the side of the sacral bone. The uterine end of the uterosacral ligament fuses with the posterior side of the main ligament and the intrapelvisal fascia tube. The broad ligament consists of a wing-like bilayered inverted peritoneum that extends from the lateral wall of the uterus to the lateral wall of the pelvis. The broad ligament boundary surrounds the fallopian tube and the round ligament, and continues to form the pelvic funnel ligament upwards.
The broad ligament surrounds the sheathed uterine blood vessels and the main ligament underneath. The two layers of the broad ligament have loose connective tissue, fat, fallopian tubes, round ligaments, ovarian intrinsic ligaments, parauterine tissue, ovarian crown, para-ovarian body, Gartner duct (ovarian coronary complex), uterus and ovarian blood vessels, lymph, and nerves. The main ligament, or ofmackenrodt, consists of dense fiber connective tissue and some smooth muscle fibers. The main ligament emanates from the lateral isthmus of the uterus and extends like a tent to the lateral pelvic wall and is fanned into the closed hole and the upper pelvis diaphragm.
This thick fibrous tissue forms a triangular diaphragm with a thick connective tissue sheath that envelops the uterine artery. The main ligament fuses medianally and lower with the uterine-vaginal fold and intrapelvisic fascia, and backwards with the uterosacral ligament. The visceral peritoneum and intrapelvis fascia are also able to support the bladder and rectum.
The anterior view of the pelvis
Lymphatic drainage
The extra-iliac lymph nodes are located above and below the extra-iliac blood vessels and can be divided into two groups, one on the lateral side of the extra-iliac blood vessel and the other behind the psoas major muscle. The distal end of the posterior lymph node is encased in the femoral sheath. These lymph nodes receive lymphatic drainage from femoral lymph nodes, external genitalia, deep abdominal wall, uterus, and internal iliac arteries. Some lymph fluid from the extra-iliac lymph nodes may flow into the intrailiac lymph nodes, but most of them enter the total iliac and para-abdominal aortic lymph nodes. Most of the lymphatic drainage that enters the extraylgenic lymph nodes comes from the vulva, but there are also drainage tracts from the cervix and under the uterus. The extra-iliac lymph nodes also receive drainage fluid from the femoral and intrailiac lymph nodes. Intrailiac lymph nodes are attached to the intrailiac vein. The intra-iliac lymph nodes are located within an anatomical triangle with three sides of the external iliac artery, the internal iliac artery, and the lateral pelvic wall. Lymph nodes in this area are of clinical importance, including lymph nodes in the femoral canal, closed-port lymph nodes, and lymph nodes adjacent to extra-iliac blood vessels. These lymph nodes receive lymph fluid from all organs of the pelvic cavity as well as lymph from the vulva, including the clitoris and urethra.
Intraperitoneal pelvic lymph nodes
The number and location of lymph nodes are not fixed, and only a significant number of lymph nodes can be found in the following locations, including the intersection of intra- and extra-iliac vessels, the closed-hole fossa near the closed-hole vessels and nerves (closed-hole lymph nodes), and the broad ligament base adjacent to the cervical ureter walking below the uterine artery (ureteral lymph nodes). Sacral median lymph nodes (sacral cape
lymph nodes) along the side of the middle sacral vessel. Lateral sacral lymph nodes can be found in the sacral holes next to lateral vessels. The intrailiac lymph nodes receive lymphatic reflux from some blood vessels in the extra-iliac lymph nodes, uterus, vagina, bladder, lower rectum, fallopian tubes, and ovaries. Its lymphatic fluid will flow into the iliac-sum and para-abdominal aortic lymph nodes.
The iliac lymph nodes are located in the middle and lateral side of the iliac blood vessel, just below the bifurcation of the aorta. Most of the iliac-total lymph nodes are located on the side of the blood vessel. In addition to draining lymph fluid within the above lymph nodes, the common iliac lymph nodes also receive lymph fluid from the cervix and upper vagina. In addition, intra-iliac, iliac, intra-gluteal, and sub-gluteal lymph nodes also flow back into the total iliac lymph nodes. pelvis
The drainage fluid of the total lymph nodes ascends into the para-abdominal lymph nodes.
Lymph nodes next to the abdominal aorta travel in tandem with the front and sides of the aorta. These lymph fluids ascend into the lumbar lymphatic trunk and eventually into the chylohydrate. The para-abdominal aortic lymph nodes receive lymph fluid from the iliac lymph nodes, abdominal pelvic organs, ovaries and fallopian tubes, and deep in the abdominal wall.
External peritoneal iliac lymph nodes
Lymphatic drainage of the internal genitalia
Innervation of the inner genitalia
The pelvic organs are mainly innervated by the autonomic nervous system. The sympathetic nerves of the autonomic nervous system originate in the thoracic-lumbar region of the spinal cord, while the sympathetic ganglia are located next to the central nervous system. In contrast, the parasympathetic nerve originates in segments of the three sacral bones in the middle of the cranial nerve and spinal cord, whose ganglions are located near the internal organs.