A 3-month-old child presents with a cheek hemangioma, a flaky hemangioma of the right cheek, about 2.5 cm in diameter, with no other abnormalities, and the initial diagnosis is infantile hemangioma.
Parents of children throw out classic triple questions: Do you need treatment? How is it treated? Are treatments safe and effective?
Infantile hemangiomas (IHs) are common benign tumors in infants and young children, most of which can resolve spontaneously, but some children's hemangiomas are incomplete or combined with different degrees of serious complications, such as disfigurement, ulcers, bleeding, etc., while hemangiomas grow in key areas such as eyes, respiratory tract, liver, etc. will seriously affect the function of the corresponding organs, and even endanger life.
Do children with hemangiomas with different sites of onset and clinical manifestations need treatment? How is it treated? How long does the treatment cycle take... It is a concern of many pediatricians.
On April 22nd, the first Infant Hemangioma Summit Forum on "Heyan Luomei New Students Jia Future" was successfully held in Chongqing, and Professor Ji Yi of West China Hospital of Sichuan University, Professor Song Xiaofeng of Children's Hospital Affiliated to Chongqing Medical University, and Professor Wang Dajia of Shengjing Hospital Affiliated to China Medical University were invited to share the pathogenesis and latest diagnosis and treatment progress of IHs, and the above questions were also answered in detail.
Highlights Sneak Peek:
New advances in the pathogenesis of IHs: therapeutic targets revealed
Expert consensus analysis: an analysis of the key process of drug treatment
Clinical treatment experiences with IHs: Typical case sharing
New advances in pathogenesis: NEW targets for the treatment of CCN1 or IHs
Professor Ji Yi of West China Hospital of Sichuan University shared the pathogenesis of IHs and the clinical treatment progress of β receptor blockers. Infantile hemangiomas are characterized by abnormal proliferation of vascular endothelial cells, and a variety of signaling pathways work together to participate in its occurrence and development, the most important of which is the VEGF/VEGFR signaling pathway.
The latest studies have shown that in hypoxia environment, the production of cysteine-rich angiogenesis inducer 61 (Cyr61 or CCN1) in hemangioma-derived endothelial cells increases significantly, inducing overexpression of vascular endothelial growth factor (VEGF), promoting endothelial cell proliferation and migration, leading to the occurrence of hemangiomas.
This finding makes CCN1 a potential new target for IHs treatments [1].
An important change in pharmacotherapy: propranolol became the first-line recommended drug for the treatment of IHs
1.
Determine whether treatment is needed based on risk assessment
The need for treatment for IHs can usually be assessed based on their disfigurement and risk of functional impairment[2], and the risk rating is shown in Table 1.
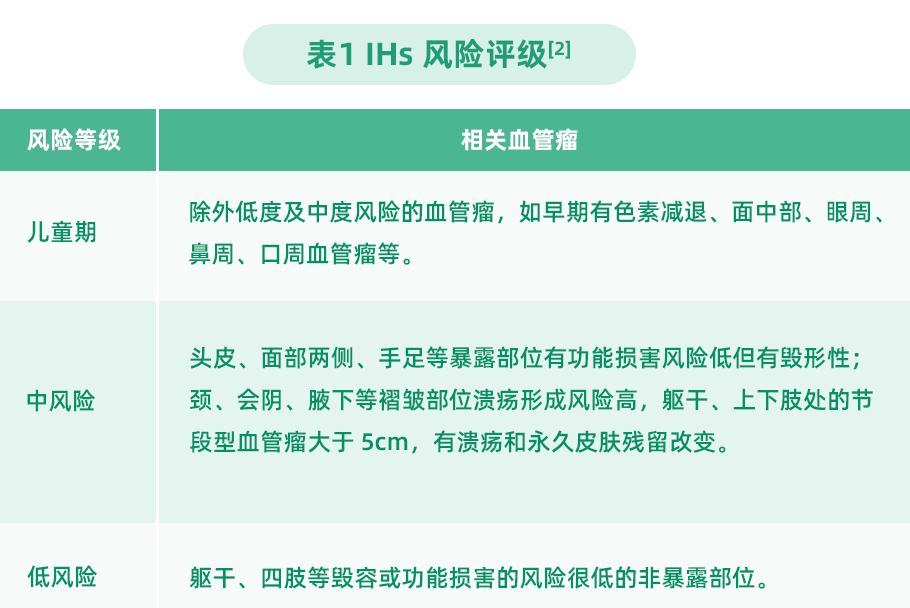
Aggressive treatment is recommended for medium- to high-risk IHs. Low-risk IHs require close observation and therapeutic intervention if they grow rapidly or if parental willingness to treat is strong.
2.
The appropriate treatment is selected according to the indications
Treatments for IHs include drugs, lasers, and surgeries, and the indications for different treatments vary slightly [3], as detailed in Table 2.
3.
Propranolol became a first-line agent for the treatment of IHs
In terms of drug therapy, glucocorticoids are traditional hemangioma clinical treatment drugs, mainly used for the treatment of systemic multiple hemangiomas [4], but their application has more adverse reactions and is currently less used.
In 2008, French scientists stumbled upon propranolol (a arrhythmia treatment) to have a good therapeutic effect on IHs, and its safety and efficacy were subsequently clinically verified, gradually replacing glucocorticoids as the first-line drug for the treatment of IHs [5-8].
At this meeting, Professor Song Xiaofeng of the Children's Hospital Affiliated to Chongqing Medical University made a detailed interpretation of the "Expert Consensus on Oral Propranolol for the Treatment of Infantile Hemangiomas"[5], which provided a high-value clinical reference for the use of propranolol for the treatment of IHs.
Indications: Oral propranolol is mainly used for the treatment of proliferative infantile hemangiomas requiring systemic therapy.
Therapeutic dose: Due to the different degrees of tolerance of the drug in children, the method of gradually increasing the amount based on the starting dose can be taken, and the child's heart rate, blood pressure, blood sugar, etc. can be monitored.
Duration: The recommended time is 6 to 12 months, and during the medication, the dose can be determined according to the degree of regression of hemangioma and the age of the child, and the dose can be reduced until the drug is discontinued.
Discontinuation: it is recommended to discontinue the drug gradually, that is, after the hemangioma completely subsides or stops resolving for more than 2 months and gradually reduce the amount of medication in the absence of changes in the condition, generally completely stop the drug at about 2 to 4 weeks, if the condition is repeated during the period, the drug can be re-administered.
At this meeting, Professor Wang Dajia of Shengjing Hospital affiliated to China Medical University also shared the clinical case of propranolol:
Two children with scrotal and perianal hemangiomas combined with rupture achieved good clinical efficacy after 5 months of oral propranolol.
Another hepatic hemangioma occurred in the fetal stage, and the pregnant woman also achieved good results after oral propranolol treatment according to medical advice.
New advances in pharmacotherapy: precise treatment of IHs in oral dosage forms
At present, propranolol is commonly used in clinical practice as a tablet, and the indications on the instructions have not yet covered infantile hemangiomas. In addition, the dose of the child needs to be adjusted according to the weight, and the oral tablets usually need to be crushed and dispensed, and the dose accuracy is not easy to control.
A foreign study found that about half of the manually cut tablets propranolol in the treatment of IHs were too much or too little [9], and the taste of the tablets was not suitable for infants and young children, and it was usually more difficult for children to take the drug, which in turn affected the clinical efficacy.
In 2014, propranolol hydrochloride oral solution was approved for marketing abroad, and IHs treatment ushered in indications for oral drugs.
A multicenter, randomized double-blind trial (n=460) study (NCT01056341) conducted abroad evaluated the efficacy and safety of oral solutions. Results Showed that 88 percent of children treated with propranolol improved at week 5, and after 24 weeks of treatment, more than 60 percent had complete or nearly complete disappearance of tumors, with no significant difference in the incidence of adverse effects from the placebo group [10].
A PK comparison of propranolol hydrochloride oral solution with tablets found that oral liquid absorption was 20 percent higher than that of tablets and that individual differences in pharmacokinetic parameters were low [11].
At present, the domestic exclusive propranolol hydrochloride oral solution (Hemeijia) has been approved for listing, which is the original research enterprise Pierre Farber Company in Greater China exclusively authorized the indication patent (patent name: β - blocker in the preparation of drugs for the treatment of hemangioma; patent number: ZL200880111892.5), and allows products produced in authorized countries [12], providing more options for the clinical treatment of infantile hemangiomas.
brief summary
While some IHs resolve naturally, they cannot simply be observed and waited for, and individualized treatment plans need to be tailored to their size, location, growth rate, complications or potential complications, and the needs of parents.
The listing of propranolol hydrochloride oral solution provides an exclusive dosage form for children with hemangioma, and the solution dosage form is conducive to accurately grasping the dose, reducing the risk of drug overdose, and the taste is more suitable for infants and young children to take, reducing parents' medication concerns, and looking forward to bringing clinical benefits to more children.
Content Planner: Wu Miaolan
Content Review: Xu Chao
Illustration source: Ash Ash
Title image source: Stand Cool Helo
bibliography
[1]. Wu P, Xu H, Li N, et al. Hypoxia-Induced Cyr61/CCN1 Production in Infantile Hemangioma[J]. Plast Reconstr Surg. 2021,147(3):412e-423e.
[2]. Luu M, Frieden IJ. Haemangioma: clinical course, complications and management[J]. Br J Dermatol. 2013, 169(1):20-30.
Zheng Jiawei, Zhao Zeliang. Research progress in evidence-based treatment of infantile hemangiomas and vascular malformations[J]. Journal of Prevention and Treatment for Stomatological Diseases, 2021, 29(11):12.
Zheng Jiawei, Wang Yan'an, Zhou Guoyu, et al. Indications for the treatment of head and neck hemangioma[J]. Shanghai Journal of Stomatology, 2007, 16(004):337-342.
Propranolol in the treatment of infantile hemangioma consensus expert group. Expert consensus on oral propranolol in the treatment of infantile hemangioma[J]. Chinese Journal of Pediatric Surgery, 2019.
Li Jianhong, Li Ping, Liu Jianzhong, et al. Retrospective efficacy analysis of oral propranolol in the treatment of hemangiomas in 120 infants[J]. Chinese Journal of Leprosy Dermatology, 2014(9):4.
[7]. Ainipully AM, Narayanan SK, Vazhiyodan AP, et al. Oral Propranolol in Infantile Hemangiomas: Analysis of Factors that Affect the Outcome[J]. J Indian Assoc Pediatr Surg. 2019, 24(3):170-175.
[8]. Kagami S, Katori T. Oral propranolol for infantile hemangiomas beyond the proliferative phase[J]. J Dermatol. 2018 \, 45(10):1199-1202.
[9]. Casiraghi A, Musazzi UM, Franceschini I, et al. Is propranolol compounding from tablet safe for pediatric use? Results from an experimental test[J]. Minerva Pediatr. 2014, 66(5):355-362.
[10]. Léauté-Labrèze C, Hoeger P, Mazereeuw-Hautier J, et al. A randomized, controlled trial of oral propranolol in infantile hemangioma[J]. N Engl J Med. 2015,372(8):735-746.
[11]. FDA: Hemangeol -ClinicalReview.
Pierre Fabre patent license.