The article comes from the Internet
Spinal injuries and lesions are very common problems in orthopedics, and familiarity with the anatomy of the spine is a basic knowledge that every doctor must master. On the basis of understanding anatomy, we can better serve patients in clinical work.
Apply dissection
(1) Basic overview
1. Overview:
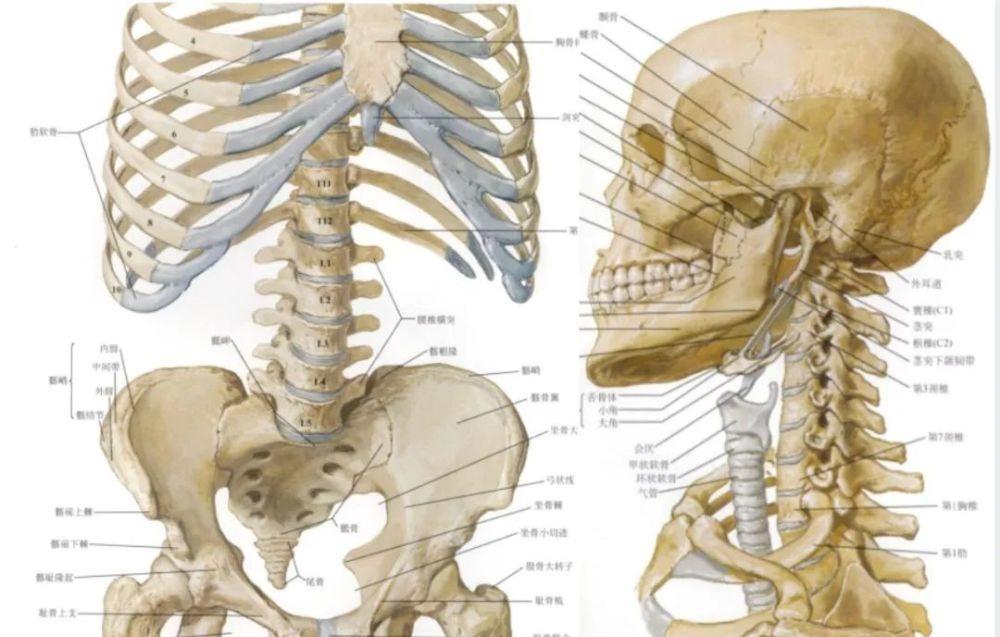
In human infancy, there are 33 vertebrae (7 cervical vertebrae, 12 thoracic vertebrae, 5 lumbar vertebrae, 5 sacral vertebrae, and 4 tail vertebrae). With age, 5 sacral vertebrae form one sacral bone, and 4 caudal vertebrae form one coccyx.
It is made by connecting ligaments, joints and intervertebral discs. The upper end of the spine supports the skull, the lower hip bone, the ribs attached to the middle, and serves as the posterior wall of the thoracic, abdominal, and pelvic cavities. The inside of the spine forms a longitudinal spinal canal from top to bottom with a spinal cord inside.
2. Features
Supports the human body
Conducted load
motion
Maintain stability
Protects the function of the spinal cord
Flexible movement of six degrees of freedom
3. Anatomical position
Crown (frontal) – Divides the body into front and back parts
Sagittal surface - divides the body into left and right parts
- Mid-sagittal surface – Divides the body into two equal parts, left and right
Cross-section (horizontal or axis) – Divides the body into upper and lower parts
Anterior view: The vertebrae gradually widen from top to bottom, with the 2nd sacrum being the widest
Side view: the neck, chest, waist, and sacral four physiological bends can be seen, the neck and waist are curved forward, and the chest and sacral curvature are convex backwards.
Posterior view: The cervical spinous process is short and bifurcated, nearly horizontal. The thoracic spinous process is slender and obliquely posteriorly downward. The lumbar spinous process is plate-like and horizontally backwards.
(2) The basic morphology and structure of the vertebrae
Physiological curvature:
Cervical bulge 20°-40°
Thoracic kyphosis 20° - 40°
Lumbar bulge 30°-50°
The sacral kyphosis is tilted
Bone tissue type:
A. Cortical bone:
Hard, mainly located on the surface of the bone
Provides bone strength, good fixation point
Harvard System
B. Cancellous bone:
Softer, mostly located inside the bone
Provides a place for strength and cell storage
Trabecular bones, spongy or honeycomb-shaped
Vertebral structure
Articular protrusions
Isthmus of the spine
Interstitial
Final plate
Cartilage endplate
Bone end plate
Bone process ring
Pedicle incision
Foramen, nerve root outlet
(3) Characteristics of each section of the vertebrae
1. Cervical spine
According to differences in anatomical morphology, the cervical spine is divided into upper cervical vertebrae (C1 to 2) and lower cervical vertebrae (C3 to 7)
The vertebrae are small, with transverse foramen, acanthous bifurcation, nearly horizontal positions of upper and lower articular processes, and large and mostly oval foramen
A. Upper cervical spine:
Cervical occipital joint – discless
Atlantoaxial (C1) – Forms joints with the skull (C0) and pivot (C2).
Atlantoaxial joints – infertile discs
Pivot (C2) – A joint that forms with C1 and C3
atlas:
It is ring-shaped and has no vertebral body
The spinous process of the 2nd-6th cervical vertebra is shorter and bifurcated at the end, while the spinous process of the 7th cervical spine is long and does not bifurcate at the end
Atlantoaxial joints:
In the atlanto-occipital junction, most of the motor functions are anterior flexion-posterior extension and lateral flexion
In the atlantoaxial joint, nearly 50% of the rotation of the head occurs here
Structure of atlantoaxial joint stability: joint capsule, anterior atlantoaxial membrane, posterior atlantoaxial membrane, mulching, atlantoaxial cruciate ligament, apical ligament of the tooth process, pterygium ligament, etc.
Pivot :
Dentate process – the rotating center of the atlantoaxial vertebrae
Transverse process - transverse foramen, vertebral arteries, radiculosis
Side blocks, larger
Articular surfaces
Spinous process (bifurcation)
B. Lower cervical spine (C3-C7)
Generally the anterior convexity is 20° -40°
Each patient is evaluated individually
All segments have interstitial discs
Joints (transition) C5-6-7
-High mobility
- Increased risk of injury
3-7 The vertebral hook on the lateral margin of the upper lateral edge of the cervical vertebral body forms a hook vertebral joint with the adjacent vertebral body, which increases the stability of the cervical spine and prevents the displacement of the upper cervical spine and the intervertebral disc.
Vertebral projection (C7)
Large, long spinous process
Anatomical markers
2. Thoracic spine
Vertebral body - T1 to T12 volume increase
Pedicle root – small in diameter
Lamina – vertically "stacked tile" arrangement
Spinous process – long, overlapping, protruding downwards
Foramen – large, reduces the risk of nerve compression
Articular protrusions
Rib transverse articular surface
The ribs and thoracic spine form the bony structure of the thoracic cage and limit the movement of the thoracic spine
Connection department
-C6 - T2
-T11 - L2
-Adjacent segments are more susceptible to damage
Floating ribs in T11 -T12
3. Lumbar spine
Vertebral body: L1 to L5 volume increase
Pedicle root: longer and wider than the thoracic spine, oval
Spinous process: horizontal, square
Transverse protrusion: smaller than the thoracic spine
Foraminal: large, but at increased risk of nerve root compression
Foramen: Large enough to accommodate the horsetail and nerve roots
The shape of the lumbar spinal canal: from top to bottom is oval---- triangular --- trifoliary
4. Sacral vertebrae
5. Sacral caudal vertebrae
6. Iliac bone
osteograft bone site itself
The rear of the iliac crest can be used for additional support and fixation of rod structures (sacroiliac fixation)
(4) Intervertebral connections
1. Ligaments:
Tough, fibrous tissue is attached to bone, cartilage or other structures
It works when the stress increases to the maximum range of movement
High elasticity protects the joints
The intervertebral arch between the arches adjacent to the vertebral vertebrae is called the intervertebral arch ligament, which is composed of elastic connective tissue and is yellow, so it is also called the yellow ligament.
Between and between each spinous process, there are interspinous ligaments and inter-traverse ligaments, respectively.
In front of the vertebrae is the anterior longitudinal ligament, the anterior edge of the large foramen of the occipital bone, the front of the lower sacrum (S1 or 2), and the front of the vertebral body and the intervertebral disc, which is thick and tough. The posterior longitudinal ligament behind the vertebral body is comparable in length to the anterior longitudinal ligament, and the part that adheres to the vertebral body is relatively narrow.
There is also a continuous supracene ligament on the tip of the spinous process, which is close to the end of the spinous process at the chest, waist, and sacrum, and is plate-like to the neck, which is a necklace ligament.
2. Spinal canal and contents
1) Spinal canal: a bone fiber tube composed of the vertebral foramen of the vertebral bone, the sacral canal of the sacral bone and the bone connection between the vertebrae, and the upper occipital bone foramen communicates with the cranial cavity, and ends with a sacral canal split hole. Its contents include the spinal cord, spinal muscular membrane, spinal nerve roots, blood vessels and a small amount of connective tissue.
Composition of the spinal canal wall:
Anterior wall: vertebral body, intervertebral disc, posterior longitudinal ligament
Lateral walls: pedicle, intervertebral foramen
Posterior wall: lamina, ligament flavum
Spinal canal morphology: There are differences in the shape and size of the segments of the spinal canal on the cross-section
Neck segment: triangular in shape
Thoracic segment: rounded, with the 4th to 6th thoracic vertebrae being the most narrowed.
Waist segment: different shapes
- The 1st and 2nd lumbar vertebrae are mostly round or oval
- The 3rd and 4th lumbar vertebrae are mostly triangular
- The 5th lumbar spine is mostly trifoliary
Spinal canal partitioning:
Depending on the shape of the spinal canal and the distribution of the contents of the spinal canal, the spinal canal is generally divided into two parts, namely the central spinal canal and the nerve root canal.
A. The central spinal canal consists of the spinal cord and its place occupied by the membrane.
B. Nerve root canal: refers to the site occupied by the spinal nerve root in the lateral part of the spinal canal, clinically known as the lateral crypt. Its anterior wall vertebral body and the posterolateral disc, the posterior wall is the superior articular process, the ligament vanthus, and the lateral wall is the pedicle and intervertebral foramen.
Relationship of the lumbar radiculocaria to the following structures:
The lumbar spinal lateral crypt is pronounced.
The disc-yellow space is the space between the intervertebral disc and the yellow ligament.
Superior articular paraforatal sulcus.
Inferior groove of the pedicle.
2) Spinal cord
Spinal cord segment correspondence to vertebrae:
The upper cervical cord (C1 to 4) is the same height as the vertebrae of the same order
The lower cervical cord (C5 to 8) and the upper thoracic cord (T1 to 4) are one vertebral body higher than the homogeneous vertebrae
The middle thoracic cord (T5 to 8) is 2 vertebral bodies higher than the homogeneous vertebrae
The lower thoracic cord (T9 to 12) is 3 vertebral bodies higher than the homometric vertebrae
The lumbar cord (L1 to 5) is flat on the 10th and 11th thoracic vertebrae
The sacral and caudal cord (S1 to 5, Co) are flat against the 12th thoracic and 1st lumbar vertebrae.
Spinal cord membrane and space of the epidermis:
Spinal indumentum (outer and inner): dura, arachnoid, and corpora
Infimbranous space (outer and inner): epidural space, subdural space, subarachnoid space
3) Spinal veins
The venous structure of the vertebral venous system is characterized by thin walls, no flaps, and many anastomosis.
Extravertebral venous plexus: extravertebral anterior venous plexus and extravertebral posterior venous plexus
Intravertebral venous plexus: the anterior venous plexus in the vertebral sphere and the plexus medial posteriorly
Intervertebral veins
Vertebral veins
Spinal veins
3. Intervertebral discs
It occupies about 1/4 of the total length of the spine, and the neck and waist are the thickest
Fibrochondral connections in the motor segments
Occurs in C2-C3 through L5-S1
Can compress, stretch and rotate movements
Maximum bloodless structure in the body
The front column bears 80% of the stress, and the middle and rear columns bear 20% of the stress
In 1983, Denis proposed the concept of three-column classification, proposing that the stability of the spine depends on the integrity of the middle column, not on the composite structure of the posterior ligament. Denis proposed a three-column classification, dividing the spine into anterior, middle, and posterior columns:
Anterior column: anterior longitudinal ligament, anterior half of the vertebral body, anterior part of the intervertebral disc.
Middle column: one-half of the posterior half of the vertebral body, posterior longitudinal ligament.
Posterior column: articular process, ligament vitis umbra, interspinous ligament, supraspinal ligament.
Nucleus pulposus:
Located in the central part
Slime jelly-like substance
High moisture content
Resists axial pressure
Fiber ring:
The outer part of the compartment
Sheet composition
Multi-layer collagen fibers
-30° tilt
- Adjacent layers are reversed
Counters shear forces in all directions
Largest vascular tissue
Nutrients come from the diffusion of the end plate
Diffusion disorders lead to disc degeneration
There are no intervertebral discs between the atlantoaxial and pivotal vertebrae, and between the sacrum and the caudal vertebrae, so there are only 23 intervertebral discs in the whole body. They are both located between the two vertebral bodies. The thoracic disc is the thinnest, and the lumbar disc is the thickest, about 9 mm.
4. Articular process joints
The articular surface of the cervical articular process is approximately horizontal.
The articular surface of the thoracic articular process is approximately coronal.
The lumbar articular process articular surface is approximately sagittal.
Occipital neck joint:
Atlantoaxial joints:
Articular surface:
Hooked vertebral joints:
Costotraum:
Lumbosacral joint:
Sacroiliac joint:
Image anatomy
1. Transverse level of the transverse pedicle:
The area where the cross-section passes: the pedicle
Main features: The spinal canal is an intact bone ring, composed of a vertebral body, a pedicle, and a vertebral arch plate
2. Transverse level of the lower part of the transvertebral body:
The area where the cross-section passes: the vertebral body under the pedicle root
Main features: The spinal canal is an incomplete bony ring, and its fracture is the upper part of the intervertebral foramen.
The structure of the upper part of the intervertebral foramen through different parts is different, the cervical segment is mainly an intervertebral vein, and the thoracic and lumbar segments are mainly spinal nerve roots.
3. Transvertebral disc transectional level:
The area where the cross-section passes: the intervertebral disc
Main features: the spinal canal is an incomplete bony ring, its disconnection is the lower part of the intervertebral foramen, the structure of the lower part of the intervertebral foramen in different parts is different, the cervical segment is mainly a spinal nerve root, and the thoracic and lumbar segment is mainly an intervertebral vein.
4. Spinal canal and contents
Epidural fat: low-density shadow
Dural sac: round or oval soft tissue density shadow. A flat CT scan does not distinguish between the dural sac, cerebrospinal fluid, and spinal cord.
Intravertebral venous plexus: located in the epidural space, not alone on CT scan, with a dotted, high-density shadow on the enhanced scan.
Spinal cord: moderate contrast in the center of the spinal canal
cerebrospinal fluid:
Low signal on T1WI;
High signal shadow on T2WI.
Spinal nerve roots: medium-signal strips or dot-like shadows.
Epidural adipose tissue:
Continuous strip or band high signal on T1WI;
Medium to high signal on T2WI.
Intravertebral venous plexus: reticulated with slightly low signal shadow.
Intervertebral foramen: Located on the anterolateral side of the spinal canal, the spinal nerve roots inside it have a soft tissue density surrounded by low-density adipose tissue
Adipose tissue filling the intervertebral foramen is highly signaled;
The spinal nerve roots that walk in it have a circular, oblong, low, or isosignal shadow
Intervertebral disc: soft tissue density shadow, CT value of 70±5HU, can not distinguish between the nucleus pulposus and fibrous rings
Nucleus pulposus: higher signal on T2WI
Fiber Ring: Low signal on both T1WI and T2WI
Sharpey fiber: Low signal on both T1WI and T2WI
Transparent cartilage plates: Low signal on both T1WI and T2WI
Ligaments of the spine:
Both the anterior and posterior longitudinal ligaments are thin and cannot be shown alone on CT.
The ligament vum is thicker (normally ≤3 mm), located on the inner side of the lamina and articular process, denser than the dural sac and epidural fat, and appears clearly
Supraspinal and interspinous ligaments also have a thin shadow of soft tissue density.
Paravertebral soft tissue: the density structure of soft tissue is presented on CT, and the CT value is about 40HU to 50HU
【Copyright Notice】This platform is a public welfare learning platform, reprinted for the purpose of transmitting more learning information, and has indicated the author and source, such as teachers who do not want to be disseminated can contact us to delete