Moments of knowledge
Bilateral thalamus infarction is relatively rare in the clinic, clinical symptoms may show a typical triad, imaging features are symmetrical venterine infarction, and most prognosis is poor. Most doctors may be impressed and obsessed with it once they encounter it in the clinic.
This article uses a case of bilateral thalamus infarction encountered in clinical work to systematically review the disease.
Let's look at the case data first
The patient is a male, 58 years old.
▌ Main complaint: unconscious, limb weakness for 8 hours.
▌ Current medical history:
The patient is unconscious without obvious precipitating causes 8 hours before admission, limb weakness, inability to hold objects, inability to walk independently, and poor speech.
No crooked corners, no headache, nausea, vomiting, no unresponsiveness, no whimsy, no gibberish, no dysphagia, no drinking cough, no convulsions, no urinary incontinence, no fall trauma.
Due to the gradual aggravation of symptoms, there was no cerebral hemorrhage in the head CT that came to our hospital for emergency treatment, and the preliminary diagnosis was "cerebral infarction" and was admitted to the hospital.
History of previous long-term alcohol consumption. Deny other significant medical histories.
▌ Admission examination:
T 35.6°C, P 110 times/min, R 17 times/min, BP 134/99 mmHg.
Superficial coma, bilateral pupils of unequal enlargement, left pupil diameter 4 mm, right pupil diameter 2 mm, bilateral refractory retardation of light, eye movement is not cooperative, the right nasolabial fold is shallow, the tongue is centered, the pharyngeal reflex is normal, and the neck is soft.
Muscle strength examination is uncooperative, limb tone is normal, bilateral tendon reflex is normal, right Side Pap sign is positive, Left Side Is Bad Sign is negative.
Heart rate 110 beats per minute, heart rhythm, no obvious murmur in the auscultation area of each valve.
Both lungs have thick breath sounds, and no obvious dry and wet sounds are heard. No significant edema was seen in both lower extremities.
Cranial magnetic resonance after admission: 1. Midbrain and bilateral thalamus infarction; 2. Bilateral parenchymal multiple ischemic lesions and softening lesions; 3. MRA shows bilateral posterior cerebral arteriosclerotic-like presentation.
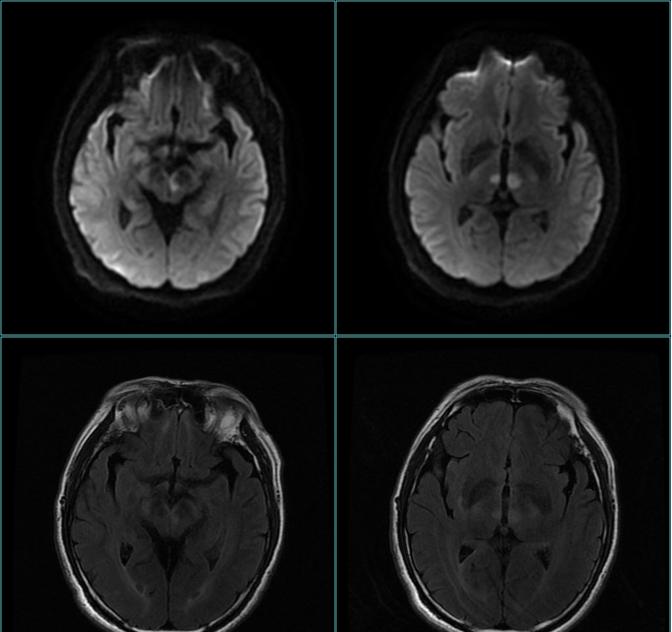
(Figure 1: Midbrain and bilateral thalamus infarction of the head MRI of the skull)
(Fig. 2. Skull MRA showing bilateral posterior cerebral atherosclerosis)
After admission, aspirin and clopidogrel hydrogen sulfate were given antiplatelet aggregation, calcium atorvastatin anti-atherosclerosis, butanphthalide to improve collateral circulation, and susannin to improve microcirculation.
After 14 days of treatment, the patient's condition improved slightly, and the physical examination: drowsiness, slightly vague speech, slightly sluggish response. Double pupils are equal to large isocircular, diameter 3mm, sensitive light response, left eye adduction is incomplete, both eyes can not move up and down, left and right diplopia, no nystagmus. Strength in the extremities is grade 5, and both lower extremities are positive for Pap signs. Both lungs have thick breath sounds, and no obvious dry and wet rales are heard. No significant edema was seen in both lower extremities.
(Figure 3: Schematic diagram of the thalamus blood supply artery, the figure originates from the network)
Details: Percheron arterial infarction
Blood supply to the thalamus is mainly supplied by four arteries: the thalamus nodule artery, the traditional thalamus artery (para-midrider), the thalamus knee artery, and the retrochoroidal artery (Figure 3).
In 1973, french scholar Percheron first reported a very rare thalamus perforation artery variant, that is, the bilateral thalamus perforation artery originated from the P1 segment of one side of the posterior cerebral artery, which was named Percheron artery (Artery of Percheron, AOP), which caused bilateral parathalamus mid-central infarction, tired or not involving the midbrain.
Percheron arterial infarction accounts for 0.1%-2% of all acute cerebral infarction and 4%-18% of acute thalamus infarction, and is a special type of cerebral infarction that is clinically uncommon in men than in women.
(Fig. 4. Schematic diagram of the anatomical type of the thalamus perforating artery, figure derived from the literature [1])
There are four anatomical types of thalamus perforation (Figure 4), of which type II.b is the vascular cause of Percheron artery infarction, when the bilateral thalamus puncture artery originates from the P1 segment of the posterior cerebral artery on one side, the artery supplies the bilateral ventral medial area of the thalamus and the upper part of the midbrain, which can lead to Percheron artery infarction when it is occluded.
Lazzaro et al. divide Percheron arterial infarction into 4 types:
Type I accounts for 43% of the case, which is a bilateral parathalamus mid-area and midbrain infarction.
Type II accounted for 38%, only bilateral parathalamus mid-center infarction, no midbrain infarction.
Type III accounts for 14%, that is, bilateral parathalamus mid-central region and anterior and midclass infarction.
Type IV accounts for 5%, that is, bilateral parathalamus mid-central area and anterior thalamus infarction, no midbrain infarction.
The typical triad of Percheron arterial infarction is impaired consciousness, vertical gaze paralysis, and memory impairment.
Impaired consciousness is due to bilateral involvement of the nucleus and central median nucleus of the medulla plate.
Vertical gaze paralysis is associated with midbrain cap involvement.
Memory impairment is due to damage to the dorsal medial nucleus of the thalamus and adjacent areas of the plate core.
Scholars at home and abroad have reported other rare symptoms including seizures, mental abnormalities, dysarthria, extraocular muscle paralysis, pupillary changes, ataxia and pseudoglobulbar palsy.
The Percheron artery is very thin and difficult to visualize on the head MRA and CTA, and can be detected by a small number of patients with superselective cerebral angiography.
Treatment is similar to other ischemic strokes, and clinical symptoms may improve to varying degrees after treatment, but most patients will still have neurological deficits and generally poor prognosis.
Early diagnosis and aggressive treatment are essential.
brief summary
In summary, clinical percheron arterial infarction is rare, and the complexity of the anatomy and the diversity of clinical manifestations are easily overlooked. This disease can leave sequelae symptoms and poor prognosis, so it should be diagnosed and treated as soon as possible to improve the quality of life of patients.
bibliography:
[1] Nicholas A,Lazzaro,B,Wright,M,Castillo,N J,Fischbein,C M,Glastonbury,P G,Hildenbrand,R H,Wiggins,E P,Quigley,A G,Osborn.Artery of percheron infarction:imaging patterns and clinical spectrum. [J]. AJNR. American journal of neuroradiology,2010,31(7):1283-9.DOI:10.3174/ajnr. A2044.
Zhang Qinli,Chen Yuying,Liu Hong,Wang Yufen,Chen Feng,Gao Zhengke. Two cases of Percheron arterial infarction[J].Chinese Journal of Internal Medicine,2018,57(6):454-456.DOI:10.3760/cma.j.issn.0578-1426.2018.06.012.
Liu Yujiao,Gan Fangzhou,Zhang Yongfeng,Zhang Qing. Percheron arterial occlusion 1 case report[J].Chinese Journal of Stroke,2019,14(9):933-936.DOI:10.3969/j.issn.1673-5765.2019.09.014.
This article was first published: Medical Neurology Channel
Author: Ice Cream
This article was reviewed: Li Tuming, deputy chief physician
【Copyright Notice】This platform is a public welfare learning platform, reprinted for the purpose of transmitting more learning information, and has indicated the author and source, such as teachers who do not want to be disseminated can contact us to delete