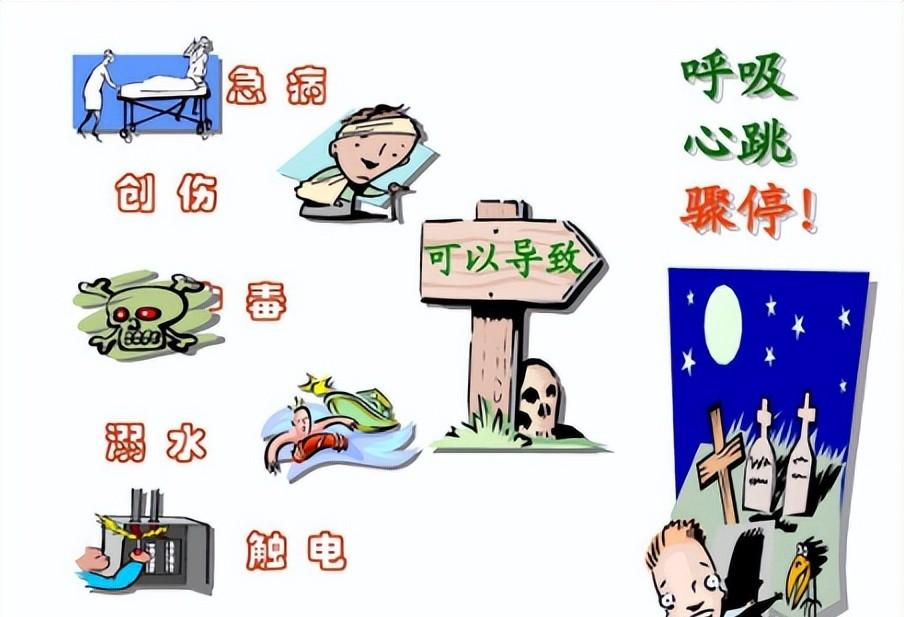
Under special circumstances, cardiac and respiratory arrest have their own characteristics, and cardiopulmonary resuscitation requires appropriate adjustment of methods and different implementations. These include: drowning, hypothermia, electric or lightning strikes, trauma, and pregnancy.
Drowning
Drowning (drowning) is the process of suffocation caused by the submerged respiratory tract by liquids, the most important resuscitation measure is to restore ventilation and oxygen supply as soon as possible, the length of hypoxia determines whether the drowning person has cardiac arrest and is related to prognosis. The method of on-site resuscitation is as follows:
1. Rescue in the water If a drowning person is found, he will be rescued from the water immediately, and the first responder must pay attention to his own safety when rescuing. Neck fixation protection should be considered if a drowning person has a significant neck injury.
2. Artificial ventilation Artificial ventilation is an important measure for the recovery of drowning, and rapid artificial ventilation without cardiac arrest can increase the chance of survival of drowning people. Artificial respiration can be performed when a drowning person is rescued ashore or is still in shallow water. Most drowning people will only inhale a small amount of water during the drowning process, and do not cause airway obstruction, only the visible foreign body in the mouth of the drowning person is properly removed before artificial respiration, and first responders do not need to routinely empty the fluid in the respiratory tract of the drowning person.
3. Chest compressions After checking the drowning person's unconsciousness and no breathing, immediately chest cardiac compressions, the compression/ventilation ratio is 30:2. When drowned in cold water, the arterial pulse of the drowning person is difficult to reach, and even if a professional emergency personnel check the carotid pulse, it should not exceed 10 seconds.
4. Other situations The treatment of drowning patients is often accompanied by hypothermia, and it should be treated according to hypothermia treatment during resuscitation. If vomiting occurs during resuscitation, the head should be tilted to one side, removed with fingers, gauze, etc. or suctioned with an aspirator.
Lightning, electric shock
Lightning strikes and eleerie shocks are electrical currents that act directly on the smooth muscles of the heart, brain, and blood vessels, as well as the thermal effect of electrical energy converted into heat energy in the body. Ventricular fibrillation and ventricular rest caused by the action of electrical current on the myocardium are the first causes of death by lightning and electric shock. Some patients cause respiratory arrest due to: (1) the suppression of the respiratory center of the bulbar through the head of the current through the head; (2) Ankylosing twitches of the septal muscles and chest wall muscles during electric shock; (3) Prolonged respiratory muscle paralysis. The characteristics of resuscitation are as follows
1. Before the rescue, the first responder first confirms that the emergency scene is safe and there is no danger of electric shock.
2. The patient breathes unconsciously, pulses, immediately starts CPR, seeks help from the EMS system, and performs electrical defibrillation as early as possible. Patients who have suffered lightning and electric shock do not have cardiopulmonary underlying disease, and immediately implement CPR, which is more likely to survive, and even needs more time than the general CPR requirements.
3. Lightning and electric shock can cause compound trauma, which can have head and neck and spine injuries. Care should be taken on protection and braking. Burning clothing, shoes, and belts should be removed to avoid further damage.
4. Patients with burns on the maxillofacial and anterior neck may have soft tissue swelling and difficulty breathing, even if there is spontaneous breathing, the tracheal intubation should be established as soon as possible to establish an artificial airway.
5. For patients with hypovolemic shock and extensive tissue damage, intravenous fluids should be quickly rehydrated, anti-shock therapy, maintain water and electrolyte balance, and maintain sufficient urine output to promote the excretion of myoglobin, potassium ions, etc. produced during tissue damage.
microtherm
Severe hypothermia (<30 °C) is accompanied by decreased cardiac output and tissue perfusion, significantly reduced body function, showing signs of clinical death, low temperature, the heart's response to drugs, pacing stimulation and electrical defibrillation is significantly reduced, therefore, the principle of treatment of cardiac arrest caused by hypothermia is to actively deal with low body temperature and carry out CPR.
(1) Heat preservation and rewarming
1. Keep warm Remove the patient's wet clothing and avoid continued exposure to low temperatures to prevent further loss of heat.
2. Rewarming The choice of rewarming method depends on whether the patient has perfusion, heart rhythm and the degree of body temperature decline.
(1) According to the body temperature of the patient center, the degree of body temperature drop can be divided into: (1) mild hypothermia (> 34 °C); (2) Moderate hypothermia (30-34 °C); (3) Severe hypothermia (< 30 °C).
(2) Rewarming mode: (1) Passive rewarming: covering the warm blanket or placing the patient in a warm environment; (2) Active external temperature: rewarming is carried out by heating devices including heat radiation, mandatory hot air ventilation and hot water bottles; (3) Active in vivo rewarming: refers to the use of heated humidification oxygen (42 ~ 46 ° C), heated intravenous infusion (43 ° C), abdominal lavage, esophageal rewarming catheter and extracorporeal circulation and other invasive techniques of rewarming.
(3) Choice of rewarming method: patients with mild hypothermia with perfusion rhythm adopt passive rewarming; Active extracorporeal rewarming is used in patients with moderate hypothermia with perfusion rhythms, and active in vivo rewarming is used in patients with cardiac arrest with severe hypothermia and no perfusion rhythm.
(b) Special methods of recovery
1. When the patient has not yet had cardiac respiratory arrest, focus on rewarming, and once cardiac respiratory arrest occurs, it is necessary to rewart while CPR.
2. When artificial ventilation, give heated (32-34 ° C) humidified oxygen mask ventilation as much as possible.
3. The effectiveness of electrical defibrillation decreases at low temperatures. When the central body temperature < 30 °C, electrical defibrillation is often ineffective. In the presence of ventricular fibrillation, an electrical defibrillation can be given immediately, if ventricular fibrillation is still present, CPR and rewarming should be continued, and the body temperature reaches above 30 °C to consider defibrillation again.
4. Patients with a low temperature time of more than 45 to 60 minutes need to be rehydrated in time for timely rehydration during the process of vasodilation and vascular bed volume increase.
trauma
The main causes of trauma-induced cardiac arrest include: (1) lack of oxygen due to severe open pneumothorax and bronchial injury or joint thoracoabdombic injury due to airway obstruction; (2) Damage to important organs such as the heart, aorta or pulmonary artery; (3) Severe head trauma affects the life center: (4) tension pneumothorax or cardiac tamponade, resulting in a sharp decline in cardiac output; (5) A large amount of blood loss leads to low blood volume and oxygen delivery disorders. Patients with traumatic cardiac arrest have a very low success rate of resuscitation:
1. CPR is implemented on the spot, and the jaw support method should be used when opening the airway to those who suspect neck injury to avoid injury to the spinal cord. If possible, a neck support is installed to fix the patient's head and neck.
2. Evaluate the patient's respiratory condition, if there is no breathing or slow breathing, immediately perform mask and balloon ventilation. If the patient's chest rises and falls are not seen during ventilation, it is necessary to pay attention to the presence of tension pneumothorax and hemothora. During resuscitation, attention should be paid to examining the patient for potential fatal injuries and treating them accordingly.
pregnancy
In the process of recovery of pregnant women, first responders should try their best to save the lives of the mother and the fetus, and at the same time, they should take into account the factors of physiological changes in the pregnant woman's pregnancy and childbirth, and the amount of heart blood and blood volume of pregnant women during normal pregnancy increased by 50%; After 20 weeks of pregnancy, when the pregnant woman is in the supine position, the enlarged visceral compressed blood vessels can reduce the amount of blood flow back to the heart and 25%, which should be taken into account when CPR.
For critically ill women, the following measures should be taken to prevent the occurrence of cardiac arrest: (1) left lying position: (2) inhalation of pure oxygen; (3) Establish intravenous access and intravenous infusion: (4) Consider reversible factors that may cause cardiac arrest in pregnant women, and actively deal with them. Pregnant women may experience cardiac arrest due to pregnancy and non-pregnancy factors, usually including overdose of drugs such as magnesium sulfate, acute coronary syndrome, amniotic fluid embolism, eclampsia, and preeclampsia, pulmonary embolism, stroke, trauma, aortic dissection, etc.
Features of on-site resuscitation are as follows:
1. Changes in the level of excitation in pregnant women can promote gastroesophageal sphincter relaxation and increase the incidence of reflux.
2. Artificial ventilation of unconscious pregnant women should be continuously pressed against annular cartilage to prevent aspiration.
3. In order to reduce the influence of the pregnant uterus on venous return and cardiac output, a cushion (such as a pillow) can be placed on the side of the patient's abdomen, so that it is tilted to the left by 15 to 30 °, and then chest compressions are performed, due to the influence of intestinal muscle elevation, chest compressions can take the upper part of the middle of the sternum.
4. Cyclic cartilage should also be pressed during endotracheal intubation to prevent aspiration. Because there may be airway edema in pregnant women, the inner diameter of the endotracheal catheter used is 0.5 to 1.0 mm smaller than that used in non-pregnant women.
5. Once a pregnant woman has experienced cardiac arrest, consideration should be given to the need for emergency caesarean section. The uterus reaches a certain size after 20 weeks of pregnancy can have the effect of hindering venous return, while the fetus is only likely to survive after 24-25 weeks of pregnancy. Therefore, pregnant women with a < 20 weeks of pregnancy should not consider emergency caesarean section, and emergency caesarean section in pregnant women at 20-23 weeks of pregnancy is beneficial to resuscitation of pregnant women, but it is impossible to save the baby's life. Emergency caesarean section at >24-25 weeks' gestation may be beneficial for saving both the mother's and the fetus's life. Emergency caesarean section should be performed as far as possible within 5 minutes of cardiac arrest in pregnant women.