Latent autoimmune diabetes in adults (LADA) refers to the type of diabetes that does not rely on insulin therapy in the early clinical stages and is characterized by slow autoimmune damage to islet β cells. Because it does not rely on insulin therapy in the early stages, it is easy to be misdiagnosed as type 2 diabetes.
The number of people suffering from LADA in mainland China ranks first in the world, and early diagnosis and timely and correct intervention are conducive to delaying the development of LADA disease and are of great significance to the implementation of the Healthy China Strategy. This article summarizes the main points of the "Chinese Expert Consensus on the Diagnosis and Treatment of Adult Occult Autoimmune Diabetes (2021 Edition)" updated in 2021 for the reference and study of medical colleagues.
01
Genetic characteristics
essentials:
- The genetic background of LADA disease has susceptibility genes for TIDM and T2DM, whose genetic characteristics are similar to T1DM.
- There are racial differences in human leukocyte antigen (HLA) susceptibility genotypes; HLA-ii. genes are the main susceptibility genes of LADA.
02
Immunological features
- Immune features of LADA include isletitis, islet autoantibodies, islet antigen-reactive T cells, etc.
- Monoglutamic acid decarboxylase antibody (GADA) is the most common islet autoantibody in patients with LADA; combined antibody screening improves LADA diagnostic rates.
03
Clinical manifestations
- The natural course of LADA can be summarized into four stages: genetic susceptibility, immune response, clinical non-insulin dependence, and clinical insulin dependence.
- Autoimmune-induced hypofunction of islet β cells is key to driving the progression of LADA and the diversity of clinical manifestations. The reduction of C peptide in patients with CONTINENTAL LADA was 3 times that of T2DM; among them, the decline of islet function in patients with high GADA titers was significantly accelerated.
- The metabolic syndrome of patients with LADA, its components, and changes in bone density is between T1DM and T2DM.
- The prevalence of kidney disease and retinopathy in LADA increases with disease progression; the prevalence and mortality of ASCVD is similar to that of T2DM.
- LADA is susceptible to autoimmune thyroid disease and routine screening for thyroid function and thyroid autoantibodies is recommended.
04
Diagnosis and typing
- According to the etiological classification, LADA is classified as a slow-progressing subtype of autoimmune T1DM.
- LADA diagnostic criteria: The following three items should be present at the same time:1) the age of onset of diabetes mellitus ≥ 18 years; (2) islet autoantibodies or islet autoimmune T cells positive; (3) not dependent on insulin therapy for at least 6 months after diagnosis of diabetes. It is worth noting that adolescents under the age of 18 also have slow-progressing autoimmune diabetes, known as juvenile occult autoimmune diabetes mellitus (LADY).
- GADA screening is recommended for all newly diagnosed patients with a phenotype of T2DM for early diagnosis of LADA.
- If cost and test availability are considered, antibody screening is recommended in patients with diabetes with high risk factors for LADA. High-risk LADA patients may have the following clinical features: family history of TIDM or autoimmune disease, non-obese body type (BMI<25 kg/m2), age of onset less than 60 years. The specific diagnostic path is shown in the following figure:
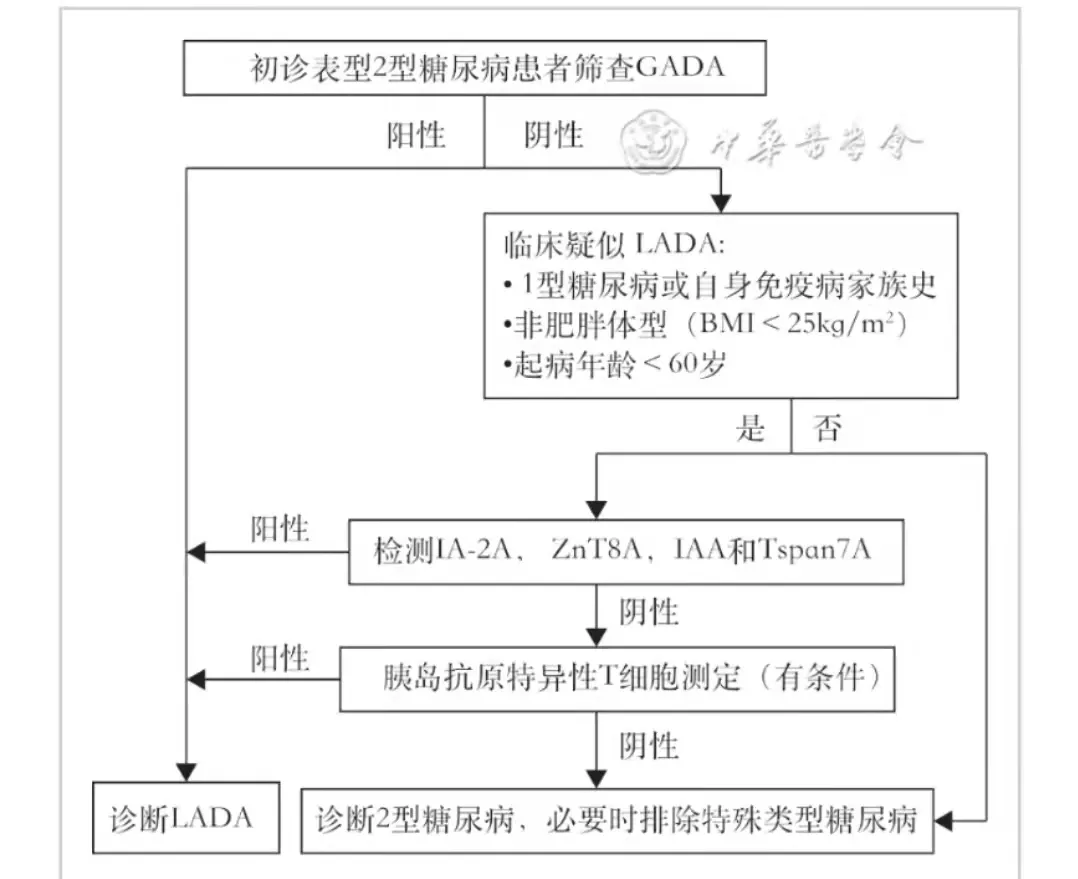
Diagnostic pathway for occult autoimmune diabetes mellitus in adults
- LADA can be divided into two subtypes according to the level of titer: LADA-1 and LADA-2. The clinical features of high titer LADA (GADA titer ≥180U/ml) are similar to classical T1DM, less likely with metabolic syndrome, called LADA-1 type, while low titer LADA is similar to T2DM, called LADA-2 type. The ratio of LADA-1 type to LADA-2 type is about 1:3 in Chinese patients.
05
Treatment and management
- The overall goals of LADA treatment: to achieve the ideal level of glucose metabolism control; to regulate the islet autoimmune response, to protect the islet β cell function; to prevent and control complications and concomitant diseases.
- LADA treatment management process: according to the C peptide level, and then according to the GADA titer and whether it is concomitant cardiac and kidney disease, hypoglycemic drugs are selected. If the C peptide < 0.3 nmol/L or GADA titer ≥ 180 U/ml, insulin therapy is recommended; C peptide ≥ 0.3 nmol/L and GADA titer < 180 U/ml, for newly diagnosed patients with HbA1c≥9%, short-term intensive insulin therapy can be used. The specific management process is shown in the following figure:
LADA Treatment Management Process
- LADA follow-up management: Since the hypofunction of LADA islet β islets in a biphasic mode of first fast and then slow, it is recommended that the Cpeptide level be checked every 6 to 12 months for patients with certain islet function. For patients with a course of more than 5 years, a comprehensive screening for complications is done at least once a year.
- Glycemic Control Goals:
- (1) HbA1c levels in PATIENTS WITH LADA are usually controlled below 7%; HbA1c is detected every 6 months for those who meet the blood glucose control standards; and HbA1c is detected every 3 months for those who change the treatment regimen or fail to meet the glycemic control standards.
- (2) For most LADA patients, it is recommended to control fasting blood glucose at 4.4 to 7.2 mmol/L, and < 10 mmol/L after meals.
- (3) The goal during pregnancy is to control blood glucose at 3.9-5.3 mmol/L on an empty stomach, 6.1-7.8 mmol/L at 1h after a meal, and 5.6-6.7 mmol/L at 2 h after a meal.
- (4) For most LADA, the recommended target range time (TIR) (3.9 to 10.0 mmol/L) >70%; for the elderly or low-glycemic high-risk LADA, the recommended TIR (3.9 to 10.0 mmol/L) > 50%; laDA co-pregnancy, the recommended TIR (3.5~7.8 mmol/L) >70%.
- Therapeutic drug selection, recommendations are shown in the figure below:
LADA recommendations for drug selection
In short, the new version of the consensus combines the LADA evidence at home and abroad, pays attention to the adoption of mainland clinical research results, and updates the diagnostic criteria, disease classification, diagnosis and treatment ideas, etc. The consensus emphasizes the importance of C peptide and GADA titers in diagnosis and treatment, and provides more reference opinions for the diagnosis and treatment of clinical LADA patients in mainland China in the future. The new version of the consensus points out that early screening and accurate diagnosis of LADA are the key to prevention and treatment, and personalized treatment is the focus of its prevention and treatment. At the same time, it is also proposed that the clinical research of LADA also urgently needs large samples and multi-center clinical trials in order to better guide clinical work and improve the level of disease prevention and treatment.
Author: Liu Xueli
Source: Endocrine Frontline
Resources
Chinese Medical Doctor Association Endocrinology and Metabolism Physician Branch, National Clinical Research Center for Metabolic Diseases. Chinese Expert Consensus on the Diagnosis and Treatment of Occult Autoimmune Diabetes Mellitus in Adults (2021 Edition)[J]. Chinese Medical Journal, 2021, 101(38):15.
Luo, Zhou Zhiguang. Interpretation of "Chinese Expert Consensus on the Diagnosis and Treatment of Occult Autoimmune Diabetes in Adults (2021 Edition)" [J] . Chinese Journal of Diabetes, 2022, 14(1): 17-20. DOI: 10.3760/cma.j.cn115791-20211126-00634.