Transferred from: Public number Laboratory Medicine
Author | Qin Yuwen Fu Zhaoqiang
Unit | Gaobo Medical (Blood Disease) Shanghai Research Center Shanghai Zhaxin Hospital of Integrated Traditional Chinese and Western Medicine
Hematopoietic stem cell transplantation (HSCT) is an effective means of treating malignant blood diseases, but patients will have some complications after HSCT treatment, of which transplant-related thrombotic microangiopathic anemia (TA-TMA) is a more serious complication, which can occur after allogeneic transplantation and autologous transplantation, mainly manifested as microvessel thrombosis, platelet (PLT) depletion, hemolytic anemia, multi-organ functional damage caused by systemic small blood vessel endothelial damage.
At present, the diagnosis of TA-TMA still lacks specific methods, and the first of several existing diagnostic criteria is the proportion of broken red blood cells (i.e., schizocytes), indicating that schizocytes are an important morphological clue for the diagnosis of TA-TMA, and peripheral blood rift red blood cell examination after transplantation has attracted more and more attention.
Case after
The patient, 15 years old, was diagnosed with aplastic anemia (acute severe) in February 2021, initiated transplant pretreatment on April 21, 2021, infused with sibling totally conjugated peripheral blood hematopoietic stem cells (male to female, O to O) on April 29, +13 days after transplantation, +13 days after transplantation, +14 days to megakaryotic implantation, +15 days to repsy to show that T cells have been fully donor chimera.
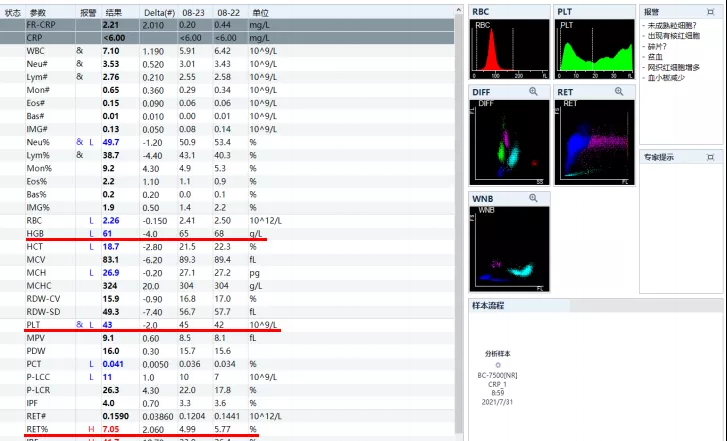
On July 30, for follow-up examination and further treatment admission, the blood routine found that the PLT was significantly reduced by 43×109/L (July 19: 100×109/L), Hb was slightly reduced by 61g/L (July 19: 71g/L), and the percentage of reticulocytes increased by 7.05%.
On 2 August, bone marrow smear showed nucleocellular hyperplasia, hypogranuity, erythroid hyperplasia with mild pathologic changes, a mild left shift of the megakaryotic maturation curve, and 2.0% of schizoid red blood cells on peripheral blood smear. Blood routine scatter plots, peripheral blood smears, and cell morphology reports are as follows:
Biochemistry suggests a significant increase in LDH and a mild increase in total and indirect bilirubin.
Other relevant tests: sC5b-9 and ADAMTS13 enzyme activity and its inhibitory antibodies were not abnormal. CMV quantitative negative, EB quantitative 2.99×103copies/mL, urine protein (1+), direct anti-human globulin test (Coombs) negative.
Case studies
Laboratory tests in the recommended diagnostic criteria for microvascular hemolytic anemia (MAHA) include: (1) peripheral hemofidocytes >1% ;(2) varying degrees of anemia; (3) evidence of intravascular hemolysis: elevated LDH, increased serum free Hb; decreased globin-binding, reticulocytosis, or compensatory hyperplasia of the bone marrow erythroids, possibly hemoglobinuria or hemosiderosis; (4) negative Coombs test; (5) thrombocytopenia.
Patients who have the first 4 laboratory tests and whose clinical findings meet the criteria for consideration for diagnosis of MAHA, of which (1) is an important prerequisite, (3) only 1 or more are present, and (5) is further supporting evidence. MAHA is mainly seen in various types of thrombotic microvascular anemia (TMA).
In this case, 3 months after transplantation (August 2), it was found that there were 2% of hydemacinocytes in peripheral blood; after transplantation, the recovery of erythroid was slow, the highest Hb was only 75g/L, the decline of erythroid was not obvious, but the PLT was significantly reduced (from 100 to 43); the LDH was significantly increased (686.9U/L), the proportion of reticulocytes was increased, the bone marrow erythroid hyperplasia was increased, and the Coombs test was negative. The above laboratory results have basically met the diagnostic criteria of TA-TMA. Patients present with post-activity fatigue, chest tightness, shortness of breath, and increased blood pressure (up to 170/100 mmHg).
Experience
Hyderocytes are caused by squeezing, destroying, or being cut by fibrin filaments through narrow microvascular when microcirculation is obstructed, usually related to blood turbulence caused by pathological changes in vascular endothelial cells. TA-TMA is one of the fatal complications of HSCT, and hydemates are important for the diagnosis of TA-TMA, so it is necessary to repeat the peripheral blood samples sent to patients after HSCT for schizocyte examination of blood smears.
Lyocytes often coexist with elevated reticulocyte percentage, bilirubin, and LDH levels, and if these four indicators are found to be elevated at the same time, they should be closely observed to prevent the occurrence of TA-TMA. In addition to cleft red blood cells, serum LDH>500 U/L and hypertension also have an early suggestive effect on the diagnosis of TA-TMA. Hypertension, proteinuria, and complement activation can be seen as early markers of renal microvascular injury and are also of interest as adjunctive diagnostic indicators of TA-TMA.
In addition, pathogenic microorganisms, especially CMV, are independent risk factors for TA-TMA, inflammation is also one of the triggers of TA-TMA, the occurrence of TA-TMA is also associated with GVHD, pre-transplantation pretreatment, HLA insufficiency donor, when the above risk factors are present, we must always be vigilant about the occurrence of TA-TMA. The latest view is that the mechanism of TA-TMA is different from classical TMA, and may be related to abnormal activation of complement or deletion of complement regulatory protein genes, which can cause endothelial cell damage. Although there is no evidence of complement activation and GVHD in this case, the diagnosis of TA-TMA is considered for hypertension, elevated total bilirubin and indirect bilirubin, proteinuria, and Epstein-Barr virus infection.
Conclusion
For suspected TA-TMA after HSCT, the proportion of PLT, Hb, rift red blood cells and hemolysis-related indicators should be closely monitored, and many laboratory results such as liver and kidney function and pathogenic microbial infection should be paid attention to, combined with early diagnosis of clinical manifestations, early treatment, and reduction of mortality.
【Reference】
[1] Shen Ti, Zhao Yongqiang, Zhou Daobin, et al. Diagnostic and therapeutic criteria for blood diseases. Beijing: Science and Technology Press, April 2018, fourth edition: 69-71.
He Yixuan, Li Sdan, Wu Runhui, et al. Progress in the diagnosis and treatment of transplant-related thrombotic microangiopathy. Chinese Journal of Experimental Hematology. 2018; 26(6):1831-1835。
Lu Wei. Recommendations of the International Committee of Hematological Standards on the Standardization and Clinical Application of Mitocytes. Clinical Laboratory Journal.2014,32(6):478-479.
Cui Chanjuan,Zhang Jie,Qiao Rui. Research progress on detection of broken red blood cells. Modern Laboratory Medicine.2016,31(2):1-4.