Venous thromboembolism (VTE) is one of the common complications in hospitalized patients. At present, the awareness of prevention in surgery is stronger than that of internal medicine, and the onset of VTE in internal medicine patients is usually insidious, and the clinical symptoms are not obvious. Therefore, it is particularly important to evaluate VTE in medical patients in a scientific manner.
1 Definitions
VTE mainly includes deep vein thrombosis (DVT) and pulmonary thromboembolism (PTE).
The former tends to occur in deep veins of the lower extremities, and may be asymptomatic or have local pain and distal edema. Proximal DVT, which occurs above the popliteal vein, is an important source of PTE emboli.
The latter is mainly a disease caused by thrombuses from the venous system or the right heart that block the pulmonary artery or its branches. It can lead to breathing difficulties, circulatory disorders, chest tightness, chest pain, etc., and even life-threatening.
2 Risk factors
VTE is developed by stasis, vascular endothelial injury, and hypercoagulant states, the three elements of Virchow. In hospitalized patients, almost everyone has a risk factor.
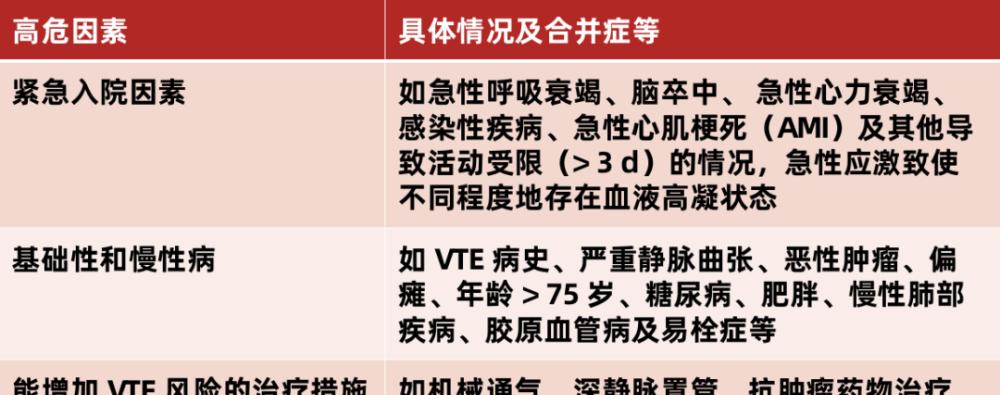
Note: Patients with two or more risk factors present at higher risk of developing VTE are at higher risk.
3 Risk assessment
Current domestic and international guidelines recommend a VTE risk assessment for all hospitalized patients in internal medicine and consider the need for VTE prevention based on the results of the assessment.
The current criteria for VTE risk assessment for hospitalized patients in internal medicine are not exactly the same, of which the Padua risk assessment model is recommended by most guidelines, and is now also used in the "Chinese Expert Recommendations for Venous Thromboembolism Prevention in Hospitalized Patients in Internal Medicine", as follows:
Padua model scoring
However, at present, there are some cases that do not apply to Chinese people, the main ones are:
One risk factor in this model was factor V Leiden mutation and prothrombin G20210A mutation, which occurred in Caucasian populations in 1% to 6%, and were very rare in Chinese populations;
There were 11 risk factors in this model, of which advanced age, AMI/ischemic stroke, obesity, and hormone therapy did not differ significantly between high-risk patients with VTE and patients with non-VTE, making it difficult to effectively distinguish between potential VTE and non-VTE patients, making it difficult to accurately predict the occurrence of VTE.
4 Value of biomarkers
1) D-dimer
D-dimers, as markers of activation of coagulation and fibrinolytic systems, indirectly reflect thrombotic activity. Has a high negative predictive value in acute VTE. Used clinically in conjunction with the Wells score, it can help rule out or confirm the diagnosis of VTE.
▲ Wells Score Numerical Table
A DVT diagnosis is excluded by a wells score of < 2 and a negative D-dimer, and a diagnosis of DVT is considered when the overall score is ≥ 2 and D-dimer is positive.
As we age, the content of D-dimer in the body will continue to increase. The current D-dimer critical values are as follows:
The degree of rise in D-dimers also suggests the degree of hemagglutination status, and the Wells score values can also be used as a predictor of future recurrent VTE. At the same time, the higher the Wells number, the higher the risk of VTE recurrence.
2) Other important biomarkers
5 Proactive prevention
Before VTE prophylaxis, a comprehensive assessment of the patient is required to control the patient's underlying disease and clarify the patient's concomitant medications. For patients with concomitant use of anticoagulants, antiplatelet drugs, thrombolytic drugs, etc., which may increase the risk of bleeding, the dose should be reduced as appropriate, or bridging therapy should be initiated as soon as possible.
1) Basic prevention
Basic prevention
Due to the peculiarities of hospitalized patients in internal medicine, active basic prevention can play a positive role.
Mechanical prevention
Mechanical prevention includes graded compression stockings, intermittent inflatable compression devices, and plantar venous pumps. It cannot be used for contraindications to mechanical prevention, and mechanical prevention alone cannot replace drug prevention.
Contraindications to mechanical prevention: severe lower extremity arteriosclerosis, congestive heart failure, pulmonary edema, lower extremity DVT (except GCS), thrombophlebitis, local severe lesions of the lower extremities such as dermatitis, gangrene, severe deformities, etc.
Patients without contraindications to mechanical prophylaxis recommend the following methods of prevention of VTE:
Contraindications to the use of anticoagulants without anticoagulation recommend the combined use of mechanical prophylaxis with pharmacoprophylaxis;
In cases of bleeding disorders or at risk of bleeding, it is recommended to use mechanical prophylaxis alone;
If the affected limb is unable or unsuitable for mechanical prophylaxis, prevention may be performed on the contralateral limb.
2) Drug prophylaxis
For hospitalized patients with risk factors, the risk of thrombosis versus bleeding must be carefully weighed:
If there are no contraindications, depending on the patient's situation, the following 1 drug may be selected for prophylaxis:
Some patients who require special prevention:
bibliography:
1. Peng Zhang, Jinbo Liu, Hongyu Wang, Research on the Application Value of Different Biomarkers in Venous Thromboembolism, Advances in Cardiovascular Disease, Vol. 42, No. 11, November 2021.
2. Ma Ping. Research Progress on Risk Assessment and Prevention of VTE in Hospitalized Patients[J]. General Nursing,2021,19(32):4496-4499.
3. Chinese Medical Association Geriatrics Branch, Chinese Expert Recommendations on Venous Thromboembolism Prevention in Hospitalized Patients (2015), Chinese Journal of Geriatrics, 2015, 34(4): 345-352.
4. China Health Promotion Fund, Recommendations for the Prevention and Management of Intra-hospital Venous Thromboembolism (2018), Chinese Medical Journal, 2018, 98(18): 1383-1388.
Curated: ly
Title image source: Stand Cool Helo
This article was first published on Lilac Garden's professional platform: Cardiovascular Time